Gastroenterologists should be aware that the symptoms of Kaposi sarcoma—the cancer that causes the characteristic skin lesions commonly associated with AIDS—can mimic those of inflammatory bowel disease.
A case study presented at the 2021 virtual Crohn’s & Colitis Congress detailed this clinical scenario and highlighted the importance of HIV screening before starting anti–tumor necrosis factor (TNF) therapy in IBD patients at risk for the infection.
“Kaposi sarcoma can mimic IBD by causing similar symptoms, such as rectal bleeding, increased stool frequency, abdominal cramping, and a similar endoscopic appearance with erythema and ulcerations within the GI tract,” said Kendall Beck, MD, an assistant clinical professor of gastroenterology at UCSF Health, in San Francisco. “Biopsies may demonstrate ‘active colitis,’ and unless Kaposi sarcoma is specifically queried, stains to identify HHV-8 [human herpesvirus-8] may not be performed.”
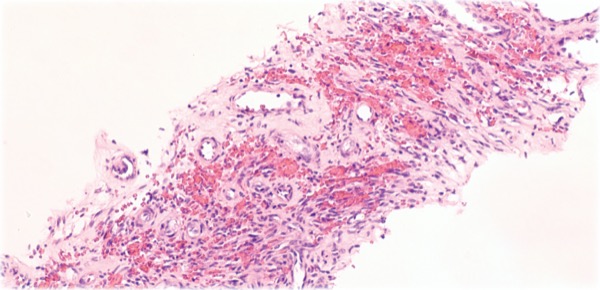
Kaposi sarcoma is a cancer of the endothelial cells that line the blood and lymph vessels. In the United States, Kaposi sarcoma most often occurs in people who are HIV-positive and immunosuppressed; the condition is associated with infection with HHV-8 and is considered an AIDS-defining illness. Kaposi sarcoma usually appears as vascular lesions on the skin and in the mouth, but it can affect any part of the gastrointestinal tract, lymph nodes and other organs.
Small studies indicate that biologics can be used safely in patients with well-controlled HIV, but no U.S. guidelines currently recommend HIV screening in high-risk groups before starting anti-TNF therapy.
Dr. Beck’s patient was a healthy, 32-year-old man in a monogamous relationship with another man, who had never been tested for HIV. He did not present with the skin lesions that typically occur with Kaposi sarcoma. However, he exhibited signs and symptoms characteristic of IBD, including bloody diarrhea, tenesmus, abdominal pain, anemia and elevated fecal calprotectin. The diarrhea had continued for a month and he had lost 15 pounds. After endoscopy and biopsies supported a diagnosis of IBD, he was treated with antibiotics and steroids intravenously, and infliximab.
A month later, the patient developed painful, purple lesions in his mouth and on his face, torso and lower extremities. A biopsy confirmed Kaposi sarcoma and he tested positive for HIV, after which he began antiretroviral therapy.
Three weeks later, new red nodules across his chest suggested worsening Kaposi sarcoma due to immune reconstitution inflammatory syndrome (IRIS). After 12 cycles of chemotherapy, the patient had no sign of residual IBD on a recent colonoscopy. Kaposi sarcoma, therefore, was likely the original diagnosis, Dr. Beck and her colleagues concluded.
While Kaposi sarcoma is relatively rare and most patients will present with characteristic skin lesions, Dr. Beck stressed that the complications this patient experienced were avoidable and said she believes that HIV screening should be standard practice before starting immunosuppressive therapy, particularly in patients who may be higher risk.
“I would advocate for screening everyone for HIV prior to initiating immunosuppression if they have not been screened recently, as HIV can exist in the absence of identifiable risk factors,” Dr. Beck told Gastroenterology & Endoscopy News. “However, it is most important to screen for HIV in patients who have at least one known risk factor for HIV infection, such as men who have sex with men or those who use intravenous drugs. We propose that all patients should be screened for common risk factors for HIV acquisition; and for high-risk patients, gastroenterologists should consider screening for HIV, in addition to tuberculosis and hepatitis, prior to immunosuppression” using anti-TNF agents.
—Adam Leitenberger
Dr. Beck reported no relevant financial disclosures.
This article is from the June 2021 print issue.