Chief of the Digestive Disease Institute
Cleveland Clinic, Cleveland, Ohio
The first study in The Regueiro Report this month is a post hoc analysis of two successful phase 3 trials, INSPIRE and COMMAND. INSPIRE showed the efficacy of risankizumab during induction as a treatment for ulcerative colitis, and COMMAND demonstrated that risankizumab also is effective as a maintenance therapy. Risankizumab inhibits the activity of interleukin-23 (IL-23).
The new study evaluates whether there is any difference in the efficacy of risankizumab in people with UC who had an inadequate response or intolerance to an advanced therapy before receiving the drug and patients who had not previously taken advanced therapies. In the study, advanced therapies included tumor necrosis factor inhibitors, Janus kinase inhibitors, anti-integrin therapies and a small number of sphingosine-1-phosphate receptor modulator therapies.
The authors found that risankizumab is safe and effective for treating UC, regardless of prior exposure to advanced therapy, which is great news for the people we treat. Assuming patients are clinically eligible, we can confidently offer risankizumab for UC, whether as a first-line therapy or in the second line and beyond if a patient has already taken an advanced therapy.
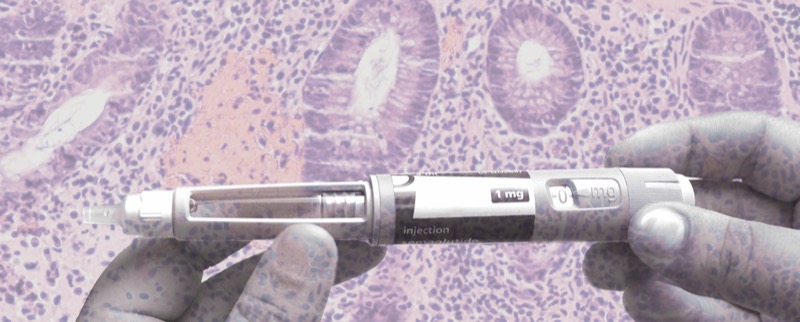
The other study is a retrospective look at the safety and effectiveness of glucagon-like peptide 1 receptor agonists (GLP-1s) in people with Crohn’s disease or UC. The introduction of GLP-1s such as semaglutide (Ozempic/Wegovy, Novo Nordisk) or liraglutide (Saxenda, Novo Nordisk) have been shown to improve diabetes mellitus and to reduce weight. Given that the GLP-1s have become increasingly common, this study evaluated the safety of these agents in patients with IBD.
This study suggests that GLP-1s are indeed safe: The authors found few adverse events in the first 12 to 24 weeks after a patient with IBD began taking a GLP-1. There also was evident weight loss and a statistically significant decline in C-reactive protein (CRP) levels.
This is a retrospective study, not a clinical trial. We need much more research investigating the intersection between IBD treatments and GLP-1s. Anecdotally, I can say that the patients with IBD who I treat often report feeling much better after they begin to take a GLP-1 and often find their gastrointestinal symptoms are improved. It is possible that treatments that target IBD and obesity at the same time could someday exist, although this is theoretical right now.
Risankizumab Efficacy and Safety
J Crohn’s Colitis 2025;19(1):jjaf005
In the induction study (INSPIRE), the subgroup with intolerance or inadequate response to advanced therapy (AT-IR) included 503 patients (48.4%) and the non-AT-IR subgroup included 472 patients, with the proportions of patients in the AT-IR subgroup similar between treatment groups (placebo, 52.3%; risankizumab, 51.2%). In the maintenance study (COMMAND), the non-AT-IR subgroup included 137 patients, and the AT-IR subgroup included 411 patients, with the proportions of patients in the AT-IR subgroup similar between the placebo (75.4%) and the two risankizumab arms (74.9% and 74.7%).
Risankizumab outperformed placebo, regardless of a patients’ experience with advanced therapies or the number of advanced therapies they had taken. Risankizumab was most effective in people who had not had an inadequate response or intolerance to a prior advanced therapy.
Safety and Effectiveness of GLP-1s in IBD
Clin Gastroenterol Hepatol 2025 Jan 30. doi:10.1016/j.cgh.2024.12.017
This is a retrospective look at the experience of 244 people with IBD (142 with CD and 102 with UC) who began to take a GLP-1, most commonly semaglutide. After 12 weeks, 203 people (83%) remained on medication. There were adverse events in 32 patients (13%), including a case of acute pancreatitis in the CD group and a case of IBD flare in the UC group.
By 12 to 24 weeks after beginning the GLP-1, average weight decreased from 102 kg (SD, 26.4) to 97.6 kg (SD, 28.0; P<0.01).
CRP levels declined in a statistically significant way in the 71 people with this data available, from a baseline of 10.1 mg/dL (SD, 16.6) to 3.0 mg/dL (SD, 6.3) (P<0.01). There also was a trend for a decline in fecal calprotectin levels in the 32 people with this lab value, from baseline 824.9 mg/g (SD, 2112.7) to 234.7 mg/g (SD, 530.8; P=0.13).
For more on GLP-1s in IBD, see “The Impact of GLP-1s on Patients With IBD.”
This article is from the May 2025 print issue.