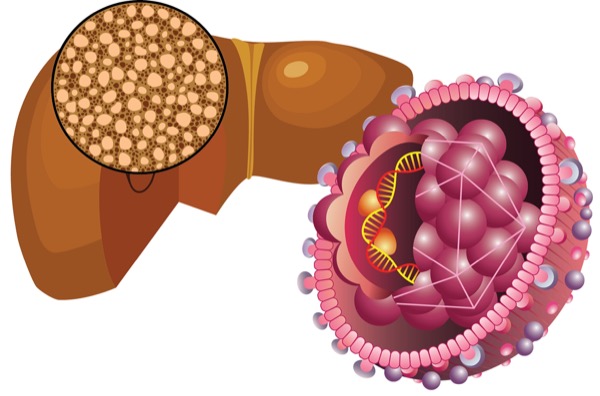
The prevalence of metabolic dysfunction–associated steatotic liver disease has increased worldwide and is particularly problematic among patients with chronic hepatitis B virus, according to new research.
Of the approximately 254 million people with HBV surface antigen (HBsAg)-positive chronic HBV, 16% to 67% may have concurrent MASLD (Lancet Gastroenterol Hepatol 2020;5[2]:167-228). The interplay between the two diseases is complex. Large cohort studies have suggested that MASLD may be protective against HBV by suppressing viral replication, yet co-occurrence may still worsen liver disease outcomes such as cirrhosis and hepatocellular carcinoma (HCC) (Front Physiol 2024;15:1347459).
The new research, from investigators at the University of Calgary, in Alberta, sheds some light on the mechanisms involved in this complicated relationship between disease states, finding that even when HBV is suppressed, coexisting MASLD leads to activation of systemic inflammatory pathways and metabolic dysregulation that may ultimately aggravate HBV-related liver fibrosis progression (J Viral Hepat 2024;31(10):582-591).
This prospective cross-sectional cohort study enrolled 53 adults aged 18 to 60 years with chronic HBV, both with and without severe hepatic steatosis and metabolic syndrome risk factors, who were treatment-naive and had no end-stage liver disease such as cirrhosis or HCC. In addition, 12 HBV-negative individuals with MASLD were recruited for immune assay control.
The investigators assessed HBV replication status using standard and novel viral biomarkers, HBV variants by deep sequencing of the HBV surface and core genes, and serum cytokine levels and ex vivo functional HBV-specific cellular immune responses to whole recombinant HBsAg and HBV core antigen, a marker of viral replication found in infected hepatocytes. They found that those with more severe hepatic steatosis showed increased peripheral systemic and Th1 cytokine levels and cellular response to whole viral proteins. Patients with metabolic syndrome and steatosis showed lower HBV markers (P<0.01), higher HBV surface diversity (P=0.02) and greater frequency of HBV variants associated with host antiviral immune escape.
“Individuals with more hepatic steatosis showed low-level viremia, unique HBV variants and systemic anti-viral immune responses, potentially impacting liver disease progression. Overall, the accumulated study data are consistent with other published work showing lower HBV viremia, including novel replication biomarkers, in CHB [chronic HBV] patients with comorbid MASLD,” wrote the researchers, led by Claudia Coffin, MD, MSc, a professor of medicine and the medical director of the University of Calgary Viral Hepatitis Clinic. “Moreover, our study data show an association between hepatic steatosis and HBV genome changes, systemic inflammation and host-antiviral specific immune responses, determined by assessment of HBV [surface] gene diversity and variants, serum cytokines and [interferon]-gamma cellular responses to recombinant HBV proteins.”
Cautioning that larger and longer studies that include patients with more diverse HBV genotypes are needed, the researchers noted their findings suggest that MASLD-associated immune–inflammatory profiles may enhance HBV-specific T-cell responses in patients with both CHB and MASLD, achieving higher rates of a functional CHB cure.
—Gina Shaw
Dr. Coffin reported financial relationships with Altimmune Pharmaceuticals, Gilead, GlaxoSmithKline, Janssen and Roche.
This article is from the December 2024 print issue.