Division of Gastroenterology and Hepatology
Medical Director, Digestive Health Center
MetroHealth
Cleveland, Ohio
In this two-part column, I highlight seven studies presented at DDW 2025. In part 1, I discuss studies on antireflux procedures and the cost-effectiveness of proton pump inhibitor versus potassium-competitive acid blocker therapy. Part 2, next month, will include studies on a new functional lumen imaging probe (FLIP) panometry–based motility classification algorithm and a new PCAB.
The first study demonstrated a resurgence in the incidence of surgical fundoplications since 2007, with clear decreased interest in magnetic sphincter augmentation (MSA), a trend that has been going on since 2018, with MSA reaching its lowest level in 2024. The second study evaluated a novel GERD device that can be used by patients postprandially to reduce episodes of gastroesophageal reflux and, consequently, symptoms. The device represents a new line of therapeutic modalities for GERD that are not invasive or pharmacologic. The third study reports on the rate of improvement in objective and subjective GERD metrics in patients who underwent gastric bypass after developing de novo GERD following sleeve gastrectomy. The study demonstrates the value of gastric bypass as a salvage treatment for patients with moderate to severe GERD post-sleeve gastrectomy. The last abstract compared cost-effectiveness of PPIs versus PCABs in patients with nonerosive reflux disease (NERD) and erosive esophagitis (EE). The authors demonstrated that cost effectiveness of PPIs was superior to PCABs, primarily due to cost. However, the study may not be generalizable globally, as the cost of PCABs may vary from one country to another.
Trends in Antireflux Surgery in the United States
DDW 2025 Presential Plenary Session, abstract 692
In a population-based study of patients with GERD, investigators used the TriNetX database to identify trends in antireflux surgery utilization between 1995 and 2024.
The investigators identified GERD patients, including those with EE, NERD and Barrett’s esophagus (BE), who underwent antireflux surgeries, including surgical fundoplication and magnetic sphincter augmentation (MSA), using CPT codes. The investigators calculated the annual incidence of antireflux surgery per 100,000 GERD patients.
Overall, there were 62,356 instances of surgical fundoplication and 1,679 of MSA between 1995 and 2024.
Over the study period, there were four distinct trends in the use of surgical fundoplication. From 1995 to 1997, the incidence decreased from 1.72 per 100,000 GERD patients to 1.32 per 100,000 (annual percent change [APC], –30.45; 95% CI, –48.33% to 0.66%). From 1997 to 2000, the incidence increased to 15.67 per 100,000 GERD patients (APC, 151.79%; 95% CI, 87.33%-203.19%). From 2000 to 2007, there was a decrease in annual incidence to 4.95 per 100,000 GERD patients (APC, –14.94%; 95% CI, –25.04% to –8.69%). From 2007 to 2024, the annual incidence once again increased, reaching 135.88 per 100,000 GERD patients in 2024 (2007-2017 APC, 33.00%; 95% CI, 27.15%-59.60%; 2017-2024 APC, 9.04%; 95% CI, –6.52% to 16.86%).
Since its first use in 2016, MSA has had two distinct trends in utilization. From 2016 to 2018, there was an increase in annual incidence from 0.18 to 7.08 per 100,000 GERD patients (APC, 411.68%; 95% CI, 83.91%-921.59%). However, from 2018 to 2024, the annual incidence decreased to 1.19 per 100,000 GERD patients (APC, –28.20%; 95% CI, –52.16% to –12.40%).
Use of antireflux surgery was more common in patients with EE or BE than in those with NERD and in those with a body mass index less than 35 versus at least 35 kg/m2. Surgical fundoplication was more common in females, whereas MSA was more common in males. MSA also was more common in those younger than 65 years of age.
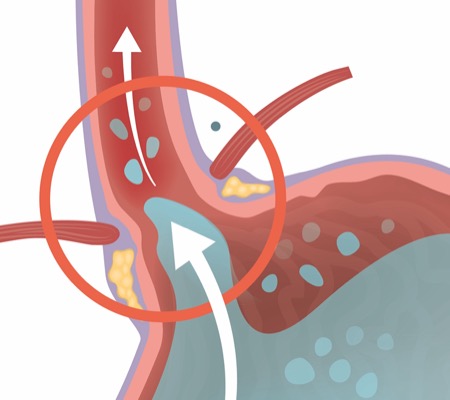
Transcutanous Electrical Stimulation System for GERD
DDW 2025 New and Novel Approaches to GERD Management Session, abstract 1151
Investigators conducted a proof-of-concept study to assess the potential efficacy of treatment with a transcutaneous electrical stimulation system (TESS) for reducing GERD symptoms.
GERD patients with heartburn and regurgitation were eligible for the study. For one week, patients did not take PPIs and kept symptom diaries. Then, the patients underwent gastroscopy and had a wireless esophageal pH capsule placed so that acid exposure time (AET) could be assessed. Patients with elevated AET (>6% of AET with pH <4) moved on to the TESS treatment phase for up to three weeks. They remained off PPIs and continued reporting symptoms in diaries.
Among the 26 patients who completed the assessment and treatment phases, 42% were female, the mean age was 49 years and the mean BMI was 25 kg/m2.
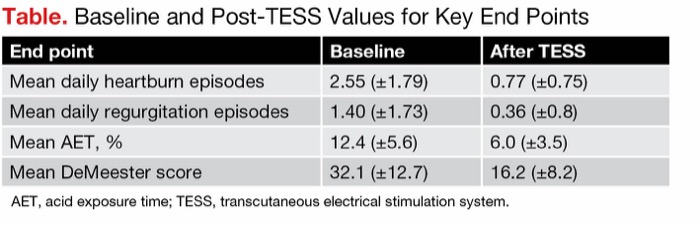
After TESS, the mean number of heartburn episodes per day, mean number of regurgitation episodes per day, mean AET and mean DeMeester score all decreased compared with baseline values (P<0.001 for each) (Table).
| Table. Baseline and Post-TESS Values for Key End Points | ||
| End point | Baseline | After TESS |
|---|---|---|
| Mean daily heartburn episodes | 2.55 (±1.79) | 0.77 (±0.75) |
| Mean daily regurgitation episodes | 1.40 (±1.73) | 0.36 (±0.8) |
| Mean AET, % | 12.4 (±5.6) | 6.0 (±3.5) |
| Mean DeMeester score | 32.1 (±12.7) | 16.2 (±8.2) |
| AET, acid exposure time; TESS, transcutaneous electrical stimulation system. | ||
The TESS also showed promising safety and tolerability, with no severe adverse events reported. Eight patients (23%) experienced mild erythema or itching, one (3%) experienced epigastric pain related to the device, and one (3%) reported feeling the electrical current.
Converting Sleeve Gastrectomy to Roux-en-Y Gastric Bypass for GERD
DDW 2025 Stomach/Bariatric/Metabolic Diseases II Session, abstract 438
Investigators at Cleveland Clinic, in Ohio, conducted a retrospective cohort study of patients who underwent conversion to Roux-en-Y gastric bypass (RYGB) due to de novo GERD after sleeve gastrectomy. They evaluated the extent to which GERD improved after the conversion, as indicated by PPI use, endoscopic assessment and pH testing, per the latest American College of Gastroenterology guidelines (Am J Gastroenterol 2022;117[1]:27-56).
In total, 117 adults who underwent conversion to RYGB between July 2004 and August 2024 due to de novo GERD post sleeve gastrectomy, and who did not have achalasia, were included in the study. Among these patients, 91.5% were female, 59.0% were white, median age at sleeve gastrectomy was 43 years, median age at RYGB was 47 years and median pre-RYGB BMI was 38.6 kg/m2.
Objective GERD improvement was seen in 45.3% of patients, with 88.7% of those improving meeting the PPI reduction criteria, 22.6% meeting the endoscopic criteria (Los Angeles Classification grade or Prague classification decrease) and 3.77% meeting the pH testing criteria. There were no differences in the baseline characteristics of those who experienced post-RYGB objective GERD improvement versus those who did not. Subjective GERD symptom improvement was reported by 88% of patients.
The subgroup of patients who had additional anatomic repair (i.e., cruroplasty and/or hiatal hernia repair) during RYGB (n=37) had a rate of objective GERD improvement (40.5%) that was comparable to that of the group without additional anatomic repair (47.5%) (P=0.615). Similarly, when stratifying by proportion of total body weight loss (TBWL) since RYGB, the proportion experiencing GERD improvement was comparable across groups (<10% TBWL [n=40], 52.5%; 10%-20% TBWL [n=40], 35.0%; >20% TBWL [n=37], 48.6%; P=0.257).
Presenter Michael Cymbal, DO, a resident at Cleveland Clinic, said the TBWL findings could indicate that “reduced intraabdominal pressure from the improvement of obesity is likely not the driver of GERD improvement.” He added that GERD improvement “may actually be the effect of the exclusion of the remnant stomach and decreased parietal cells.”
Cost-Effectiveness of PPIs Versus PCABs for GERD
DDW 2025 New and Novel Approaches to GERD Management Session, abstract 1152
A multicenter team of researchers modeled the cost-effectiveness of PCABs relative to PPIs for the treatment of EE and NERD. A decision analysis tree was the basis for the model inputs, with branches for treatment (PCABs vs. PPIs), diagnosis (NERD vs. EE LA grade A/B vs. EE LA C/D), short-term response (symptom improvement at four weeks for NERD, healing at eight weeks for EE) and long-term response (maintenance at six months). In addition, those initially taking PPIs who did not have short-term response were able to step up to PCABs after failed PPI dose optimization.
{RELATED-VERTICAL}Model inputs were based on the published literature, including clinical trial data, as well as publicly available data on drug costs and productivity costs due to symptoms.
The primary outcome was quality-adjusted life-years (QALYs) and secondary outcomes were costs and incremental cost-effectiveness ratios (ICERs).
Among both NERD and EE patients, treating with PCABs cost $3,240 more over six months versus PPIs. This corresponds to an ICER of over $144,000 per QALY. The superior cost-effectiveness of PPIs was consistent when looking at NERD or EE only.
According to the investigators, the cost-effectiveness of PPIs was mainly driven by the greater costs of PCABs, despite the latter’s marginally better efficacy in most treatment scenarios.
In a sensitivity analysis that modeled 100,000 scenarios of a range of plausible values for each model input, the PPIs were found to be more cost-effective nearly 72% of the time.