TORONTO—Esophageal stricture commonly is managed with endoscopic dilation. However, it is not the only effective intervention. In a presentation at the 2023 ISDE World Congress, Ronnie Fass, MD, MACG, the director of the Division of Gastroenterology and Hepatology at MetroHealth Medical Center and a professor of medicine at Case Western Reserve University, in Cleveland, shared seven expert tips for management of routine esophageal stricture.
1. Assess patients’ nutritional status
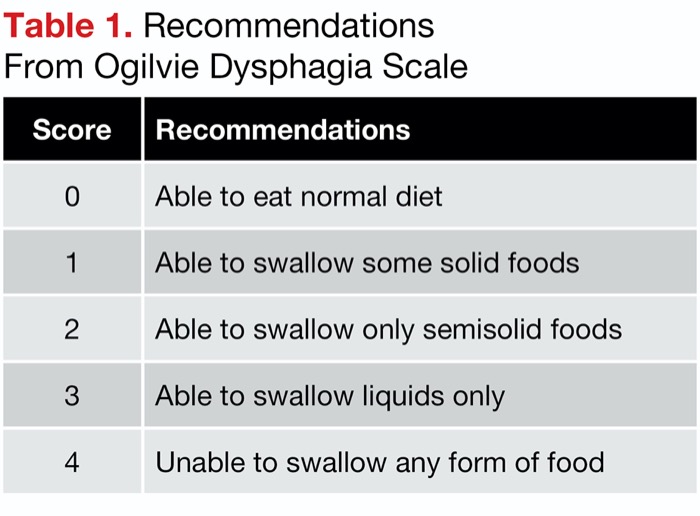
Esophageal stricture can lead to obstruction that may compromise nutritional consumption, Dr. Fass noted (Nutrients 2022;14[22]:4819). Patients commonly experience dysphagia for solids and, in severe cases, for liquids. He recommended assessing dysphagia with the Ogilvie Dysphagia Scale, which, he said, “tells you what the patient can and cannot eat.” The scale ranges from 0 to 4, where zero represents no dysphagia and 4 is a total inability to swallow (Table 1). Clinicians can use this scale to assess patients’ level of dysphagia and guide them in their food choices, Dr. Fass said.
| Table 1. Recommendations From Ogilvie Dysphagia Scale | |
| Score | Recommendations |
|---|---|
| 0 | Able to eat normal diet |
| 1 | Able to swallow some solid foods |
| 2 | Able to swallow only semisolid foods |
| 3 | Able to swallow liquids only |
| 4 | Unable to swallow any form of food |
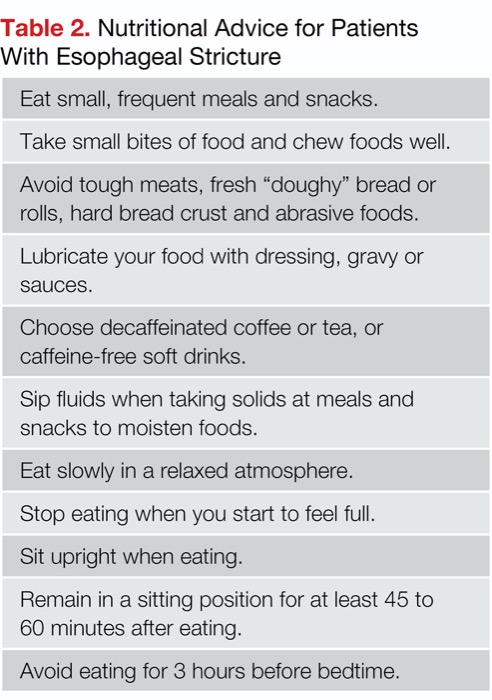
2. Provide basic nutritional instructions
Patients with esophageal stricture can benefit from simple advice that will make it easier for them to maintain nutrition, Dr. Fass said. He offered suggestions to share with patients, such as “take small bites of food and chew the food very well” (Table 2). In severe cases, Dr. Fass noted, patients may require a liquid diet or a percutaneous endoscopic gastrostomy or percutaneous endoscopic gastrojejunal tube.
| Table 2. Nutritional Advice for Patients With Esophageal Stricture |
| Eat small, frequent meals and snacks. |
| Take small bites of food and chew foods well. |
| Avoid tough meats, fresh “doughy” bread or rolls, hard bread crust and abrasive foods. |
| Lubricate your food with dressing, gravy or sauces. |
| Choose decaffeinated coffee or tea, or caffeine-free soft drinks. |
| Sip fluids when taking solids at meals and snacks to moisten foods. |
| Eat slowly in a relaxed atmosphere. |
| Stop eating when you start to feel full. |
| Sit upright when eating. |
| Remain in a sitting position for at least 45 to 60 minutes after eating. |
| Avoid eating for 3 hours before bedtime. |
3. Refer to dietitians
Esophageal strictures can lead to weight loss, and physicians may consider a referral to a dietitian, who can work with patients to develop a high-calorie diet that can help them regain lost weight or prevent weight loss.
4. Avoid certain medications
Some medications can worsen strictures, regardless of the cause of the stricture, because they may produce inflammation in the strictured esophagus, Dr. Fass said. The list of drugs to avoid includes nonsteroidal anti-inflammatory drugs, aspirin, bisphosphonates, and any medications associated with pill-induced esophagitis.
5. Use PPIs in GERD when appropriate
Noting that “7% to 23% of patients with untreated reflux esophagitis will develop peptic stricture” (N Engl J Med 2022;387[13]:1207-1216), Dr. Fass said the incidence of peptic stricture dramatically decreased after the introduction of PPIs in the early 1990s (Am J Gastroenterol 2006;101[12]:2685-2692). “This class of drugs has reduced complications of GERD to the extent that most gastroenterologists rarely see patients with peptic stricture, and most cases of peptic stricture are due to causes other than GERD,” Dr. Fass said.
Research has demonstrated that twice-daily administration of a PPI produces better results than once-daily administration, he noted. Dilation alone is not sufficient when treating these patients. “You need to address the inflammatory process in order to improve outcomes for this group.”
Dr. Fass also stressed the importance of prescribing a medication that patients can tolerate. Some individuals may tolerate an orally disintegrating tablet better than a pill or standard tablet.
6. Treat the cause
GERD is only one possible cause of strictures. Other causes include eosinophilic esophagitis and skin disorders that may involve the upper esophagus (e.g., epidermolysis bullosa, epidermolysis bullosa acquisita, pemphigus vulgaris, cicatricial phempigoid and lichen planus). Dr. Fass noted that “all of these conditions have an inflammatory process underlying their stricture.” He emphasized that while dilation is an important intervention, “physicians should treat the underlying inflammation prior to dilating whenever possible.” In eosinophilic esophagitis, the goal is to normalize eosinophil count before dilation; in skin disorders, patients should be treated with topical or systemic steroids or retinoids.
7. Consider autodilation
Autodilation with a bougie dilator “is still an option for a small number of patients where other interventions are unable to solve the structural problems,” Dr. Fass said. “Patients can be trained to perform autodilation at home prior to a meal and are able to better enjoy their diet.”
Dr. Fass encouraged gastroenterologists to “make use of the full armamentarium available for the treatment of esophageal strictures.”
—Alexis Campbell
Dr. Fass reported no relevant financial disclosures. He is a member of the Gastroenterology & Endoscopy News editorial board.
{RELATED-HORIZONTAL}