CHICAGO—On average, surgeons are much less likely than gastroenterologists to detect adenomas during routine screening colonoscopy, according to a VA data set.
Based on the lower relative adenoma detection rate (ADR), the disparity “highlights potential opportunities for quality improvement,” according to study investigator Andrew J. Gawron, MD, PhD, a gastroenterologist at the VA Salt Lake City Health Care System and an assistant professor at the University of Utah, also in Salt Lake City.
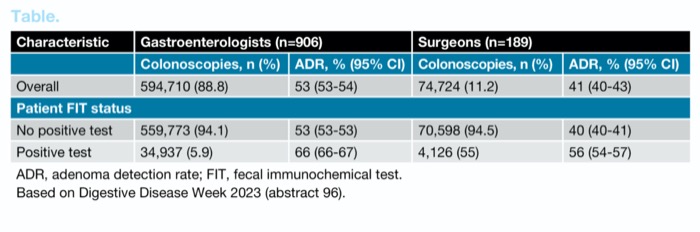
The study analyzed 669,434 colonoscopies performed by 1,095 unique providers between October 2018 and September 2022. Although gastroenterologists greatly outnumbered surgeons (906 vs. 189) and performed 88.8% of the procedures, more than 70,000 colonoscopies performed by surgeons were available for comparison.
The higher overall ADR for gastroenterologists relative to surgeons (53% vs. 41%) was dwarfed by the difference between GIs and surgeons missing an ADR threshold of at least 30, which is a guideline-recommended level of proficiency. Among surgeons, the failure to exceed the ADR threshold was nearly 10 times greater (20.1% vs. 2.1%), according to data presented by Dr. Gawron at Digestive Disease Week 2023 (abstract 96).
When the researchers divided the study population, surgeons performed less well than gastroenterologists across all of groups, Dr. Gawron reported.
Regardless of who performed the colonoscopy, higher ADR rates were achieved in male patients than in female patients, in whites than in non-whites, and in patients who did relative to those who did not have a prior positive fecal immunochemistry test (FIT) (Table). However, surgeons performed less well than gastroenterologists in all of these groups, Dr. Gawron reported.
| Table. ADRs of Gastroenterologists and Surgeons Across Subgroups | ||||
| Characteristic | Gastroenterologists (n=906) | Surgeons (n=189) | ||
|---|---|---|---|---|
| Colonoscopies, n (%) | ADR, % (95% CI) | Colonoscopies, n (%) | ADR, % (95% CI) | |
| Overall | 594,710 (88.8) | 53 (53-54) | 74,724 (11.2) | 41 (40-43) |
| Patient FIT status | ||||
| No positive test | 559,773 (94.1) | 53 (53-53) | 70,598 (94.5) | 40 (40-41) |
| Positive test | 34,937 (5.9) | 66 (66-67) | 4,126 (55) | 56 (54-57) |
| ADR, adenoma detection rate; FIT, fecal immunochemical test. Based on Digestive Disease Week 2023 (abstract 96). | ||||
In those with a prior positive FIT, for example, the greater ADR favoring gastroenterologists (65.9% vs. 57.3%; P<0.001) was statistically significant. For males, the ADR was 55% and 42% for gastroenterologists and surgeons, respectively. For females, it was 37% and 27%, respectively.
By five-year stratifications starting at age 45, the ADR was in most cases 10% or higher for gastroenterologists than surgeons, reaching 13% higher for patients 70 to 75 years of age.
Rectifying Poor Performance
In credentialling guidelines issued by the American Society for Gastrointestinal Endoscopy, the recommended number of colonoscopies before assessment of competency is 275. In comparison, the Society of American Gastrointestinal and Endoscopic Surgeons requires fewer than 100 colonoscopies before an assessment for competency.
Differences in training may or may not be a factor explaining the higher ADR rate among GIs relative to surgeons in the study, but Dr. Gawron said he was not implying with these data that surgeons are unqualified to perform colonoscopies. He noted that the majority of surgeons met the quality criterion for adequate screening.
Rather, Dr. Gawron emphasized the importance of measuring quality markers and rectifying poor performance so that performance measures are met regardless of who is performing the colonoscopy. He noted that surgeons are needed to meet the demand for screening colonoscopies, particularly in areas of the country that are underserved by gastroenterologists.
Protocols to measure quality performance and address deficiencies are common at many centers, said Trilokesh Kidambi, MD, the director of the colon cancer screening program at City of Hope Hospital, in Duarte, Calif.
Quality assurance is an ongoing process at his institution, Dr. Kidambi told Gastroenterology & Endoscopy News. “We have report cards distributed quarterly as part of our joint program between our gastroenterologists and our medical center’s quality improvement program,” he said, noting that several measures, not just ADR, are tracked.
But he emphasized that the goal extends beyond just meeting minimal standards, describing a proactive strategy for remaining current. “We also have regular journal clubs highlighting recent articles on colonoscopy quality, and we incorporate our endoscopy nurses and technicians into these discussions to build a culture of high-quality, evidence-based care,” he said.
Assessments of quality metrics for colonoscopy also are performed and reported quarterly at the East Bay Center for Digestive Health, in Oakland, Calif., where Neil H. Stollman, MD, practices gastroenterology and performs screening colonoscopy. Again, several quality metrics other than ADR, such as withdrawal times and cecal incubation rates, are followed.
“There is variation [in performance] as there would be in any large cohort of doctors, and we have absolutely identified outliers and worked with them to improve skills,” Dr. Stollman said. “We can improve outlier performance.”
In regard to the VA study, Dr. Stollman speculated that colonoscopy volume also might be a variable between the GIs and surgeons. Although volume figures were not provided for GIs versus surgeons, Dr. Stollman said if it is true that the GIs in this study were performing more endoscopies, the conclusion “should not really be that GIs are better at colonoscopies than surgeons but that doctors who do more colonoscopies are better than those who do less.”
—Ted Bosworth
Drs. Gawron, Kidambi and Stollman reported no relevant financial disclosures.
{RELATED-HORIZONTAL}