A recent study examining the transmission of prophylactic antibiotic-resistant bacteria from the anesthesia work area may shed new light on the connection to the occurrence of surgical site infections (SSIs).
While it was previously established that reducing microbial transmission through the anesthesia work area is important for preventing SSIs (Anesth Analg 2012;114[6]:1236-1248; JAMA Netw Open 2020;3[3]:e201934), researchers took a closer look at these studies to understand the mechanics of how bacterial transmission can translate to these infections (J Hosp Infect 2023;134:121-128).
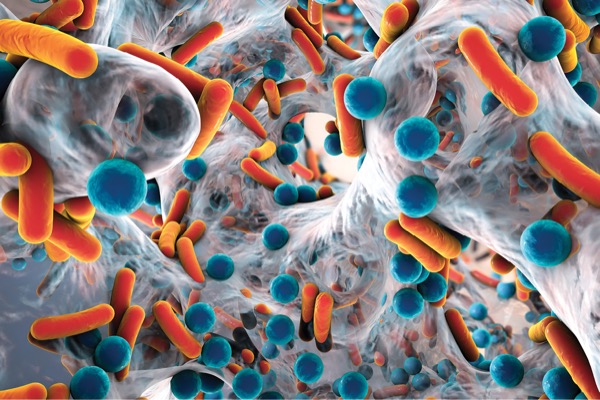
As an example, transmission might include the detection of the same Staphylococcus aureus pathogen from the nose of one patient to the anesthesia machine during the case and then to the IV lumen during the second case in the OR that day.
“Transmission, or movement, of S. aureus among anesthesia work area reservoirs has been directly linked to surgical site infection development by molecular techniques in many prior studies,” said lead author Randy Loftus, MD, an associate professor of anesthesia at Carver College of Medicine at the University of Iowa, in Iowa City. “In this study, we looked at the relative importance of transmission of isolates resistant to the prophylactic antibiotic employed for surgery.”
To understand how transmission of prophylactic antibiotic-resistant bacteria from the anesthesia work area might affect the risk for SSIs, the researchers retrospectively analyzed S. aureus isolates from previously collected samples. The data included information about what prophylactic antibiotic was administered, whether transmission occurred, and whether the patient subsequently developed an infection.
The researchers tested the archival isolates for susceptibility to the prophylactic antibiotic used and evaluated the association between SSI development and transmission of antibiotic-susceptible or -resistant isolates.
Overall, S. aureus transmission occurred in 20% of cases, of which 20% were resistant to the prophylactic antibiotic administered. The risk for developing an SSI was 11% with transmission of antibiotic-susceptible S. aureus and 18% with transmission of resistant S. aureus. In contrast, patients who did not have S. aureus transmission had an SSI risk of only 2%.
“Increasing antibiotic resistance is associated with an increase in worldwide mortality. This is in part related to the fact that antibiotic-resistant infections are more difficult to treat. Thus, transmission of more resistant isolates would be expected to be associated with an increase in infections,” Dr. Loftus said.
Treating the groups with no transmission, transmission of a susceptible isolate, and transmission of a resistant isolate as 0, 1 and 2, the researchers used exact logistic regression and found that the odds of an SSI increased by 3.59 with each unit increase (95% CI, 1.92-6.64; P<0.0001).
In their analysis of transmission events, the researchers identified 14 “transmission stories” describing the transmission of resistant S. aureus isolates. In every case, transmission was somehow linked to an intraoperative reservoir, most often the anesthesia machine, anesthesia personnel or the patient.
“In clinical studies, there are up to 300 hand hygiene events during a case, including 30 during anesthesia induction alone. The whole job is you touch the patient, and then you go to the anesthesia cart for your drugs. You touch the patient, and you go to the machine. The thing is, you cannot perform hand antisepsis 300 times,” said co-author Franklin Dexter, MD, PhD, the director of the Division of Management Consulting in the Department of Anesthesia at Carver College of Medicine.
What can anesthesia personnel do to help prevent transmission of bacteria and thus prevent SSIs? The researchers offer the following advice: Follow the pillars of infection control (Curr Environ Health Rep 2015;2[3]:226-235).
Dexter noted five key areas for decontamination. “You have the nose, the skin of the patient, your own hands, the machine and the cart, and then you have the intravenous lumen. Do you need to do all of them? Probably yes.”
For decontamination, he recommends nasal povidone iodine and using chlorhexidine wipes in the patient’s groin and axilla. Hand antisepsis is also critical.
“You need to have the hand antisepsis on the IV pole between you and the patient. That matters in terms of positioning to use it,” Dr. Dexter said.
Before and during the case, he also recommended wiping down the environment, including the anesthesia machine and cart, with a microfiber cloth soaked in quaternary ammonium and alcohol, and he suggested using disinfecting caps to clean IV ports.
“Most infections are related to transmitted isolates that are sensitive to the prophylactic antibiotic employed,” Dr. Loftus said. “Thus, the overarching goal should be to prevent transmission, or movement between anesthesia work area reservoirs of isolates that are both sensitive and resistant.”
—Jenna Bassett, PhD
Dr. Loftus reported research funding from Georgia-Pacific Manufacturing, Sage Medical Inc., B. Braun, Draeger, Surfacide and Kenall; has one or more patents pending; and is a partner of RDB Bioinformatics, LLC, which owns OR PathTrac. In addition, he has spoken at educational meetings sponsored by Kenall and B. Braun. Dr. Dexter provides consultations to corporations and hospitals, including several infection control companies.
Originally published by our sister publication Anesthesiology News
{RELATED-HORIZONTAL}