CHICAGO—Of several potential advances in the treatment of gastrointestinal cancers presented at the 2023 annual meeting of the American Society of Clinical Oncology, four new trials may help change the way several GI cancers are treated. In two trials, investigators looked at approaches to personalize surgery treatment plans for colon and pancreatic cancers. Two other trials evaluated targeted therapies for HER2-positive biliary tract and colorectal cancers, but more research is needed to determine which patients would be best suited to these treatments.
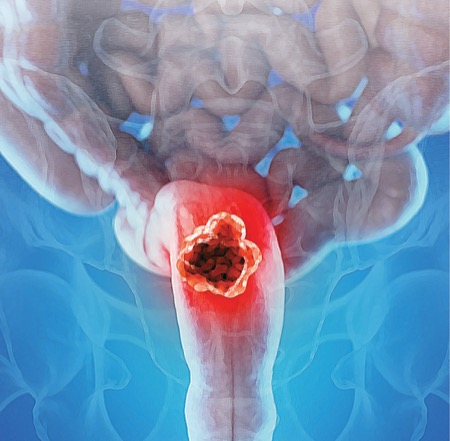
Neoadjuvant Chemo Vs Upfront Surgery For Colon Cancer
In the phase 3 NeoCol trial, neoadjuvant chemotherapy was found to be as good as but not superior to oncologic surgery for colon cancer, but it had the potential for fewer complications, according to lead investigator Lars Henrik Jensen, MD, PhD, an associate professor and a consultant at the Danish Colorectal Cancer Center South and the University Hospital of Southern Denmark, in Vejle.
To evaluate whether up-front chemotherapy could be more effective than up-front surgery for preventing dissemination of micrometastases and modifying toxicities, the investigators randomized 248 patients at nine centers in three countries (abstract LBA3503). Adults with locally advanced colon cancer were eligible if they had T4 or T3 cancer with an invasion depth of at least 5 mm and no metastases or lymph node involvement. In the standard treatment arm, up-front surgery was followed by either three cycles of CAPOX (oxaliplatin and capecitabine) or four cycles of FOLFOX (oxaliplatin and 5-fluorouracil every two weeks). The experimental arm received one of these regimens before moving on to resection. The choice of chemotherapy regimen in both groups was based on guideline recommendations in the context of disease stage and patient characteristics.
There was no significant difference between the two groups after two years of follow-up in the primary outcome of disease-free survival (DFS) or overall survival (OS) (P=0.95 for all).
Most complications and adverse effects were less frequent in the group receiving up-front chemotherapy, including ileus (3% vs. 8%), anastomotic leakage (2% vs. 8%) and sensory neuropathy (2% vs. 5% during follow-up). Dr. Jensen also reported that fewer patients developed lymph node involvement (48% vs. 59%) by the end of two years.
Based on the tumor downsizing associated with neoadjuvant chemotherapy and the trend in this group toward less chemotherapy exposure and toxicity, the investigators concluded that offering chemotherapy first and resection second “could be considered a viable treatment option” for locally advanced colon cancer.
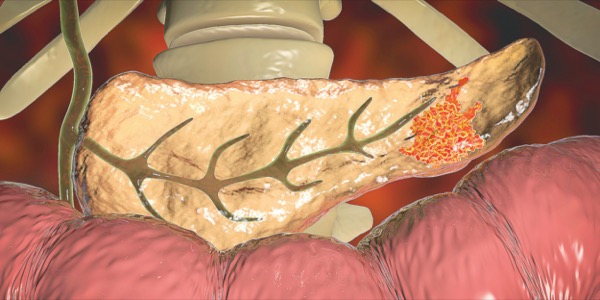
Minimally Invasive Sx For Locally Advanced Pancreatic Cancer
In this noninferiority trial in patients with locally advanced pancreatic cancer, outcomes were again at least as good with the nontraditional approach—minimally invasive surgery—as with traditional open surgery.
The study, called DIPLOMA, was the first randomized trial to compare the two approaches directly, according to lead investigator Mohammad Abu Hilal, MD, the director of surgery at Fondazione Poliambulanza Hospital Institute, in Brescia, Italy.
In the study, 258 patients with resectable pancreatic cancer were enrolled and randomized at 35 participating centers in 12 countries (abstract 4163). For participants randomized to the minimally invasive approach, laparoscopic or robotic procedures were permitted. The open procedures were consistent with current standards. Patients and pathologists were blinded to the assignment. The investigators set the predefined noninferiority margin at –7%.
The primary outcome was tumor clearance at the microscopic level (R0, <1 mm free margin). This was achieved in 73% of the evaluable patients in the minimally invasive surgery group and 69% of the evaluable patients in the open surgery group. The difference was statistically significant (4% difference; 90% CI, –6% to 14%; P=0.039).
The rates of median lymph node yield (22 vs. 23; P=0.86) and intraperitoneal recurrence (41% vs. 38%; P=0.45) did not differ significantly, nor did median OS (40 vs. 39 months; P=0.94) or median DFS (44 vs. 45 months; P=0.88).
Serious adverse events were numerically but not significantly lower in the minimally invasive group (18% vs. 22%; P=0.45). The healing process was not more rapid in the minimally invasive surgery arm: time to functional recovery was five days in both groups.
Dr. Abu Hilal said this study does not establish minimally invasive surgery as superior to open surgery for efficacy or for outcomes, but it does establish “the oncological validity of this approach.” Noting that the minimally invasive approach is already common, if not a standard, at many surgical centers where resections of pancreatic malignancies are performed at a high volume, Dr. Abu Hilal said this randomized trial now provides evidence-based support for this approach.
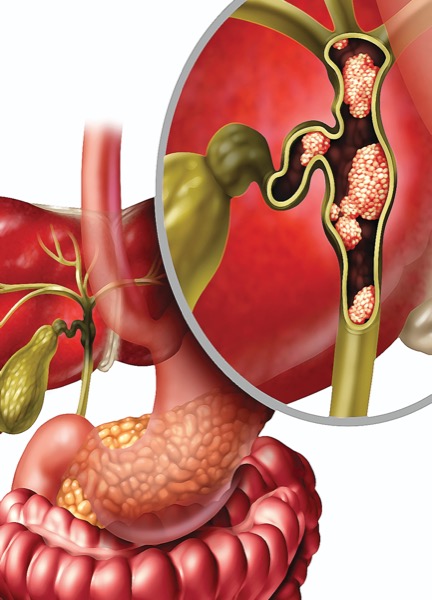
Targeted Rx for HER2-Amplified Unresectable Biliary Tract Cancer
In a pivotal phase 2b trial, the investigational bispecific monoclonal antibody zanidatamab was found to be highly active, producing clinically meaningful benefit in patients with HER2-amplified, treatment-refractory, unresectable biliary tract cancer.
“All subtypes of [HER2-amplified] biliary cancer seemed to benefit from treatment,” reported investigator Shubham Pant, MD, MBBS, a professor in the Department of Gastrointestinal Medical Oncology at The University of Texas MD Anderson Cancer Center, in Houston.
The multinational study, called HERIZON-BTC-01, enrolled 87 patients with biliary tract cancer who were naive to anti-HER2 agents but had progressed on previous chemotherapy. Activity was evaluated in two study cohorts, one with 80 patients who had HER2 immunohistochemistry (IHC) scores of 2+ or 3+ (cohort 1) and another with seven patients who had IHC scores of 1+ or 0 (cohort 2). All patients received a 20 mg infusion of zanidatamab on days 1 and 15 in each 28-day cycle. The primary end point was objective response rate. The data were published in Lancet Oncology (2023;24[7]:772-782) simultaneously with the ASCO presentation (abstract 4008).
In cohort 2, no activity was seen, producing an objective response rate of 0. In contrast, 41.3% of patients in the cohort with an IHC score higher than 1 had an objective response, including one complete response (1.3%). In addition to the partial response rate, disease control (no progression) was achieved in an additional 20%. The median time to an objective response was 1.8 months (range, 1.6-5.5 months). The median progression-free survival (PFS) was 5.5 months.
Diarrhea was the most common toxicity, but it was largely manageable, according to Dr. Pant, who reported serious adverse effects in 8% of patients and a low rate of toxicity-related discontinuations.
Dr. Pant noted that randomized trials are planned.
Trastuzumab Deruxtecan Highly Active In HER2-Positive Metastatic CRC
The antibody drug conjugate trastuzumab deruxtecan (T-DXd) appears to be moving closer to an indication for HER2-positive CRC, according to new phase 2 data in patients with metastatic disease.
In the DESTINY-CRC02 trial, rates of activity were substantial, reported investigator Kanwal Pratap Singh Ragav, MBBS, MD, an associate professor in the Department of Gastrointestinal Medical Oncology at The University of Texas MD Anderson Cancer Center, in Houston.
The study enrolled patients with RAS wild-type or RAS mutant metastatic CRC that was IHC positive for HER2 (2+ or 3+), evaluating T-DXd at a dose of 5.4 mg/kg in 80 patients and 6.4 mg/kg in 40 patients (abstract 3501). The median prior lines of chemotherapy among those enrolled was three. The primary end point was objective response. Secondary end points included duration of response and PFS.
A confirmed objective response was observed in 37.8% (95% CI, 27.3%-49.2%) of patients treated with the lower dose and 27.5% (95% CI, 14.6%-43.9%) of those given the higher dose. All were partial responses. Among those with IHC 3+ HER-2 positivity, the objective response reached 46.9% with the lower dose. Response rates were higher among patients who had RAS wild-type than RAS mutant CRC receiving either dose. (Lower dose: wild-type, 39.7%; mutant, 28.6%; higher dose: wild-type, 32.4%; mutant, 0%).
Both DOR (5.5 vs. 5.3 months) and median PFS (5.8 vs. 5.5 months) were slightly longer in patients receiving the lower dose.
Along with better rates of activity with the lower dose of T-DXd, adverse events were less common than with the higher dose, according to Dr. Ragav. This outcome included a lower rate of serious adverse events (24.1% vs. 30.8%) and grade 3 or higher adverse events (49.4% vs. 59.0%).
These data in CRC add to other evidence presented at the 2023 ASCO meeting that suggests that HER2-positive solid tumors in late stages respond to T-DXd regardless of anatomy. In the DESTINY-Pan Tumor 02 trial (abstract LBA3000), which enrolled patients with any advanced or metastatic cancer expressing HER2, the objective response rates were 50% or higher for almost all cancer types. The most notable exception was pancreatic cancer, which had a response rate of zero.
Similar to other HER2-expressing tumors, CRC is also highly responsive to T-DXd. Dr. Ragav called this drug “a promising strategy” and worthy of additional trials to identify optimal candidates.
—Ted Bosworth
Dr. Abu Hilal reported financial relationships with Ethicon and Medtronic. Dr. Jensen reported financial relationships with 2CureX, Bristol Myers Squibb, Incyte and Merck. Dr. Pant reported financial relationships with Arcus Biosciences, Astellas, Boehringer Ingelheim, Bristol Myers Squibb, Elicio, Ibsen, Janssen, Lilly, Mirati, NGM, Novartis, Pfizer and Xencor. Dr. Ragav reported financial relationships with AbbVie, AstraZeneca, Bayer, Daiichi Sankyo, Eisai, Guardant Health, HiberCell, Innovent, Janssen, Merck, Roche, UCB and Xencor.
{RELATED-HORIZONTAL}