Sessile serrated polyps pose a unique challenge to endoscopists. They are easy to miss, can be incompletely resected and are thought to become cancerous more quickly than conventional adenomas, according to experts.
“The sessile serrated polyps [ssPs] are kind of like the new polyps on the block,” said Robin B. Mendelsohn, MD, the clinical director of the Gastroenterology, Hepatology, and Nutrition Service and co-director of the Young Onset Colorectal and Gastrointestinal Cancer Center at Memorial Sloan Kettering Cancer Center, in New York City. “We’re pretty familiar with the routine colon polyps, which are tubular adenomas,” Dr. Mendelsohn noted. In contrast, “sessile serrated polyps are these flat polyps that can be found anywhere in the colon but are often found on the right side of the colon, and they’re difficult to see and spot.
“Even when you do see them, a lot of times they might be bigger than you initially think,” Dr. Mendelsohn said. “We do know that these … progress to colon cancer, just on a different pathway than the tubular adenomas.”
ssPs are now estimated to produce about 15% to 30% of sporadic colorectal cancers, but they were rarely detected before 2010, noted Seth Gross, MD, the clinical chief of gastroenterology and hepatology at NYU Langone Health in New York City, during a presentation at the 2022 New York Society of Gastrointestinal Endoscopy annual course. Instead, ssPs were lumped with other nonconventional adenomas and considered hyperplastic polyps, and existing guidelines typically suggested that the group as a whole was benign, Dr. Gross added.
Pathologic Continuum
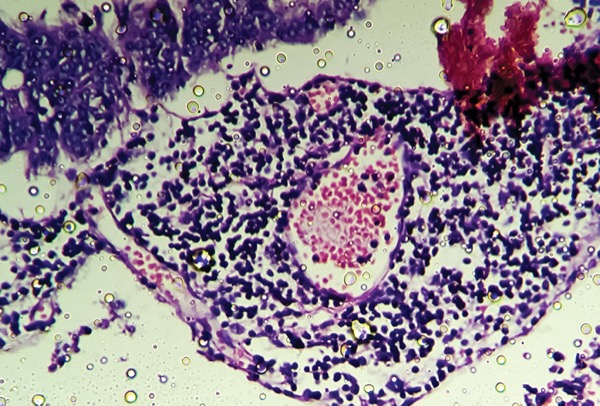
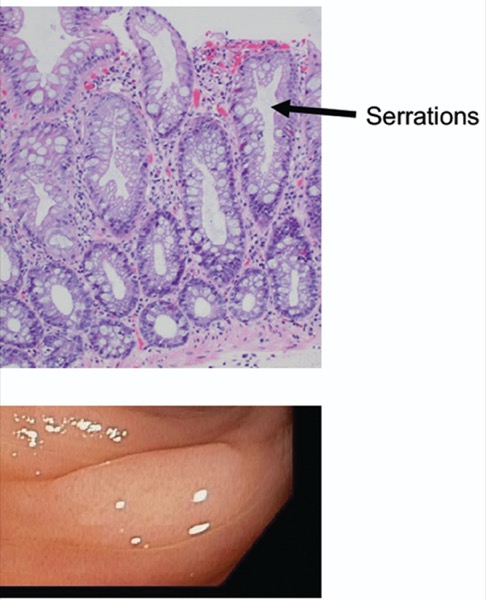
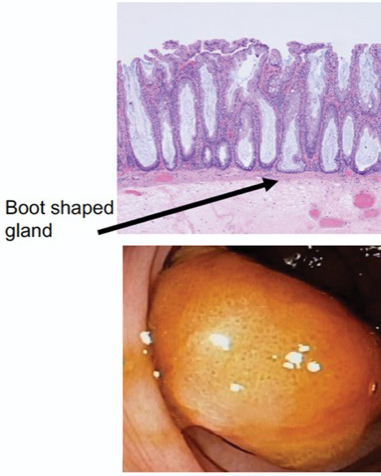
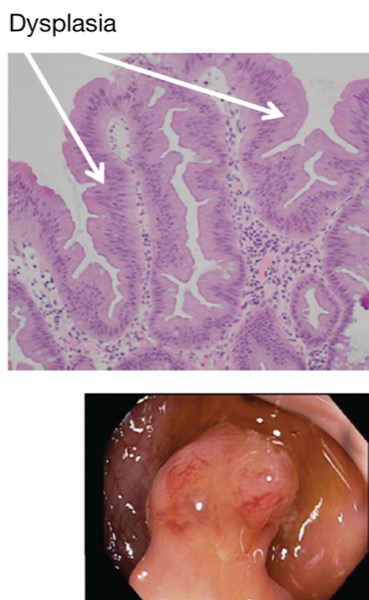
Today, serrated polyps are classified as hyperplastic polyps (HP), ssPs, or traditional serrated adenomas (TSA) (Table). HPs, which make up 90% of serrated polyps, have no dysplastic potential (Figure 1). ssPs, which make up about 10% of serrated polyps are proximal, flat and pale, and have dysplastic potential (Figure 2). TSAs are very rare, pedunculated and distal, and are already dysplastic (Figure 3).
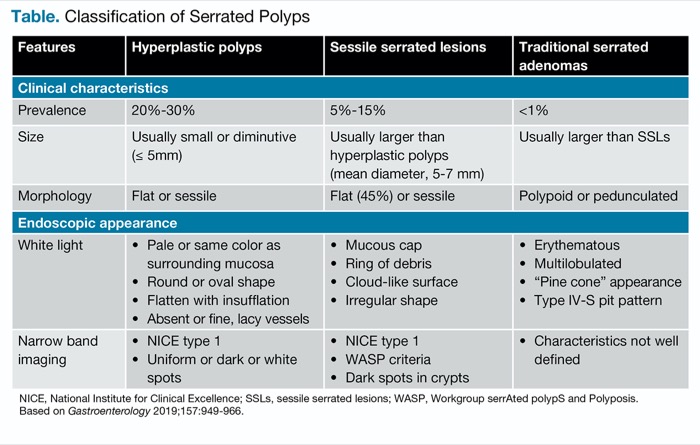
| Table. Classification of Serrated Polyps | |||
| Features | Hyperplastic polyps | Sessile serrated lesions | Traditional serrated adenomas |
|---|---|---|---|
| Clinical characteristics | |||
| Prevalence | 20%-30% | 5%-15% | <1% |
| Size | Usually small or diminutive (= 5mm) | Usually larger than hyperplastic polyps (mean diameter, 5-7 mm) | Usually larger than ssLs |
| Morphology | Flat or sessile | Flat (45%) or sessile | Polypoid or pedunculated |
| Endoscopic appearance | |||
| White light |
|
|
|
| Narrow band imaging |
|
|
|
| NICE, National Institute for Clinical Excellence; ssLs, sessile serrated lesions; WASP, Workgroup serrAted polypS and Polyposis. Based on Gastroenterology 2019;157:949-966. | |||
HPs and TSAs probably exist along a continuum, and categorization is likely to vary between pathologists, according to Dr. Gross. In terms of clinical significance, HPs that are 1 cm or larger are equivalent to ssPs, and those 5 to 9 mm may be misdiagnosed ssPs. Small rectosigmoid HPs are not clinically significant, Dr. Gross said.
Dr. Gross also discussed long-term CRC risks, and noted that for polyps 1 cm or larger, serrated polyps carry risks for CRC that are similar to those associated with advanced adenomas (HR, 4.2; [95% CI, 1.3-12.3] vs 3.3; [95% CI, 2.1-5.2], respectively) (Gut 2015;64[6]:929-936).
Better Detection Needed
Those increased risks should encourage gastroenterologists to put emphasis on improving detection of ssPs, according to Dr. Gross. “We talk about the adenoma detection rate and seeing improvements among endoscopists, but we don’t hear physicians say what their ssA [sessile serrated adenoma] detection rate is. I think ssA detection is another measure physicians should track and aim to improve,” he said.
To improve ssP detection rates, he suggested various strategies, including an adequate withdrawal time, diligently washing debris on the colonic mucosa, and closely inspecting as much of the colon wall surface area as possible.
“Sessile serrated polyps are easily missed, due to subtle features seen on colonoscopy.” He said the features can include a mucous cap, a nodular surface, draping over colon folds and “a rim of debris.” In addition, they may “obscure the blood vessel seen on the colon wall, [be] dome shaped, and [have a] red or pink color very close to normal colon wall color,” Dr. Gross told Gastroenterology & Endoscopy News. When uncertain, he said he injects dye to improve visualization.
The consequences of missed ssPs could be significant. Each 1% increase in proximal ssP detection is associated with a 7% decreased risk for interval cancer, whereas a 1% increase in adenoma detection is associated with a 3% decreased risk for interval cancer, Dr. Gross said.
“So clearly there is a difference between adenoma and serrated polyp pathways to colon cancer,” Dr. Gross said. “Clinically it is believed the sessile serrated polyp has a shorter timeline to developing colon cancer compared to traditional adenoma,” he said.
Detection Assisted by AI
Dr. Mendelsohn suggested that artificial intelligence can be a useful supplement during colonoscopy to help find subtle lesions. “Even before we had AI, I always told everyone in the room, keep your eyes out, because the more eyes, the more helpful. There’s a known miss rate, even in the best of hands. We don’t usually miss big things, but the more eyes on it the better, and I think that AI just acts as another help,” she said. Sometimes AI can help identify a lesion, she said, and sometimes “if you see something and then the patient moves or something happens and you lose it, [AI] can help you find it again.”
Dr. Mendelsohn said that gastroenterologists “need to be open to new techniques” to help increase their adenoma detection rates as well as their ssP detection rates, which, she added, “should emerge as part of our quality indicators.”
Beyond deteection, it’s also important to achieve a complete resection, but that can be difficult, and recurrences do occur. The CARE (Complete Adenoma Resection) study found an incomplete resection rate of 10.1% for adenomas and 31.0% for ssPs (P=0.043) (Gastroenterology 2013;144:74-80). Options to reduce incomplete resection include use of endoscopic mucosal resection (EMR) (see box).
“The problem with these lesions versus a traditional adenoma is that you can’t always appreciate the borders,” said Dr. Gross. “You think you got it, but you don’t know for sure. So I encourage you, before you do any resection, to really make sure that you know where these edges are. The larger the lesion, the more likely we risk an incomplete resection of sessile serrated lesions.”
—Jim Kling
{RELATED-HORIZONTAL}