University of Kansas
School of Medicine
Kansas City
Endoscopic submucosal dissection and detection of proximal colon polyps are the two major themes of this month’s installment of “Sharma’s Endoscopy Insights.” I’ll discuss three studies exploring hemostasis management during ESD, same-day discharge after ESD and increases in proximal colon adenoma detection rates (ADRs).
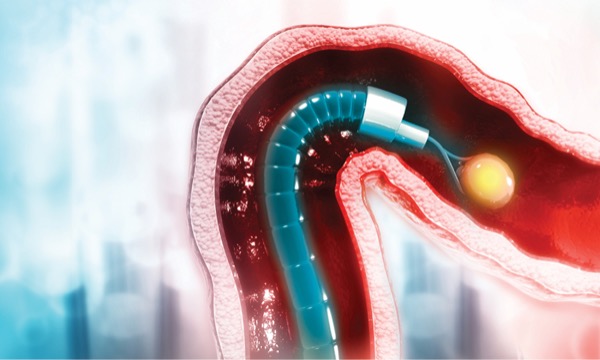
ESD is increasingly being used for minimally invasive resection of early-stage gastrointestinal cancer. However, one of its challenges is intraprocedural bleeding. This can be controlled with the waterjet function and coagulation grasper forceps. Alternatively, a study conducted in Japan evaluated the utility of a synthetic peptide that can be used during the procedure to achieve hemostasis.
Many patients undergoing ESD remain in the hospital postoperatively, but a new study showed that might not be necessary for the majority of patients. In a prospective, U.S. multicenter cohort of patients who underwent ESD for esophageal, gastric or colorectal neoplasia, investigators identified risk factors associated with admission versus same-day discharge. Complications, including bleeding and perforation, affected less than 3% of patients. Critically, risk stratification indicated that the majority of patients could be discharged after ESD, helping to optimize resource utilization.
Finally, polyps in the proximal colon often can be flat and difficult to detect. Providers use numerous techniques to increase the ADR in the proximal colon, including retroflexion, distal attachments on the colonoscope, chromoendoscopy or a second examination. This randomized controlled trial showed a significant increase in the ADR in the proximal colon using a second-view examination. These findings suggest we all should be doing a second view of the proximal colon during a routine colonoscopy.
Peptide Solution to Reduce Bleeding
Am J Gastroenterol 2022;118(2):276-283
In a multicenter, open-label, randomized controlled trial in Japan, researchers evaluated the safety and efficacy of the synthetic self-assembling peptide TDM-621 (3-D Matrix) as a treatment for blood oozing during gastric and rectal ESD. No previous clinical studies have fully examined the efficacy and safety of TDM-621 in the gastroenterology setting.
Conducted between August 2017 and August 2019, the study included 227 patients with gastric and rectal epithelial tumors undergoing ESD who experienced bleeding from an unknown source during the procedure. The researchers randomized patients into a control group in which hemostasis was achieved with hemostatic forceps and an intervention group in which hemostasis was achieved with TDM-621, followed by coagulation hemostasis with hemostatic forceps.
The mean number of times coagulation was achieved with hemostatic forceps was significantly reduced in the TDM-621 group (one time) compared with 4.9 times in the control group. The results also showed that the rate of hemostasis achieved with only TDM-621 was 62.2%. The mean dose of the peptide solution was 1.75 mL. There was no significant difference in serious adverse events between the two groups (TDM-621, 6.2%; control, 5%). Overall, the investigators found that TDM-621 was effective and safe for use during gastric and rectal ESD to treat blood oozing.
Same-Day ESD
Gastrointest Endosc 2023 Jan 29. doi:10.1016/j/gie.2023.01.042
In a post hoc analysis of a multicenter study, researchers from the United States and Canada evaluated the safety and feasibility of same-day discharge after ESD. They also examined the factors associated with admission.
The researchers prospectively evaluated 821 people undergoing ESD from April 2016 to April 2021, with the majority of procedures targeting the colorectum (465 colorectum, 240 esophagus and 126 stomach; median polyp size, 44 mm). They found that 71% of patients were discharged the same day. Of 243 patients admitted, 223 (92%) were discharged after 24 hours or less of observation.
Admission was more likely after procedures performed by endoscopists with an ESD volume of less than 50 cases (odds ratio [OR], 2.1; 95% CI, 1.3-3.3; P=0.001) and with procedure times longer than 75 minutes (OR, 13.5; 95% CI, 8.5-21.3; P<0.0001). Having lesions in the upper gastrointestinal tract instead of the colon (OR, 1.7; 95% CI, 1.1-2.6; P=0.01), invasive cancer (OR, 1.9; 95% CI, 1.2-3.1; P=0.01), and adverse events (OR, 2.7; 95% CI, 1.5-4.8; P=0.001) were other significant factors that could lead to admission.
These findings can be used to help evaluate the risk for each patient and plan for their post-procedure recovery, the researchers noted, and same-day discharge can be safe and feasible for many patients.
Taking a Second Look at the Proximal Colon
Clin Transl Gastroenterol 2023;14(1):e00557
In this prospective, single-center randomized controlled trial, researchers in China looked at whether a second examination of the proximal colon could increase the ADR.
The study enrolled 840 patients undergoing colonoscopy at the Third People’s Hospital of Jingdezhen, Jiangxi Province, from June 2021 to June 2022. During colonoscopy, after the physician completed the first, standard, forward-view examination of the proximal colon, they opened an envelope that indicated whether the patient had been randomized into the intervention or the control group. If they were in the intervention group, the physician inspected the proximal colon again.
Proximal colon ADR was significantly higher In the intervention group than in the control group (35.7% vs. 25.2%; P=0.001). Whole-colon ADR also was higher in the intervention group (44% vs. 34%; P=0.003).
A second examination may allow for a more comprehensive mucosal inspection from a different angle, the investigators wrote, and this simple technique should be considered during routine colonoscopy.
— Compiled and written by Jillian Mock
Dr. Sharma is a member of the Gastroenterology & Endoscopy News editorial board.
{RELATED-HORIZONTAL}