CHARLOTTE, N.C.—Distal cap–assisted endoscopic mucosal resection was safe and effective for removing stubborn nonlifting or adherent colorectal polyps in a retrospective study presented at the 2022 annual meeting of the American College of Gastroenterology.
Submucosal fibrosis can be induced by prior endoscopic manipulation, including biopsy, tattoo, snare sampling and previous attempts at polypectomy, noted investigator Scott Douglas, MD, a third-year gastroenterology fellow at Penn State Health Milton S. Hershey Medical Center, in Hershey, Pa. This fibrosis will cause a “negative lift sign” and make subsequent resection or EMR more difficult, he explained. It can also increase the risk for recurrence, especially after failed polypectomy.
“This is a problem that has plagued therapeutic endoscopists who receive these referrals,” Dr. Douglas said. “A number of techniques have been developed to facilitate the removal of these fibrotic or adherent polyps, but current methods are limited by lack of efficiency and cost concerns.”
He and his co-investigators employed a technique called distal cap–assisted EMR (EMR-DC). “We think EMR-DC is a safe, efficient and effective way of managing fibrotic and non-lifting polyps that have been previously manipulated,” Dr. Douglas said, noting the technique is “an especially nice option in terms of cost concerns. At our institution, the $23 cap is the only extra thing you need [in addition to standard EMR equipment],” he said.
How EMR-DC Is Performed
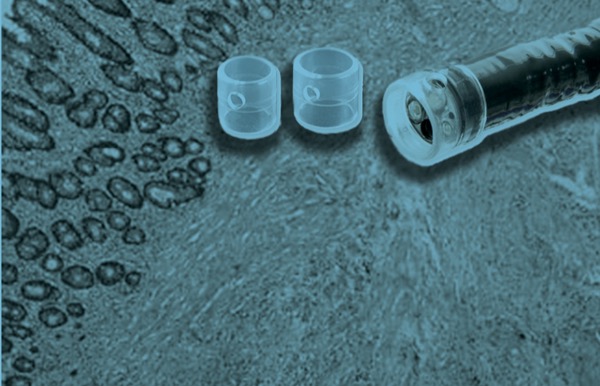
EMR-DC uses an adult- or pediatric-sized colonoscope and a standard clear distal attachment cap. The cap is positioned 3 to 4 mm from the face of the colonoscope, “which is a critical detail in that it prevents you from obtaining too much tissue and creating a deep muscle injury,” Dr. Douglas explained.
Describing the procedure, he said, the endoscopist should first assess the lesion, making sure there are no signs of malignant submucosal invasion, then proceed with the submucosal lift.
If the lesion lifts appropriately, Dr. Douglas said, it can be resected with standard EMR technique. For parts that do not lift, the cap-assisted technique can be employed by “situating the snare over the tissue you want to capture and suctioning it up through the snare into the cap,” he explained. “This causes what we call ‘endoscopic blue out.’ Then you close the snare, let go of your suction, advance your catheter, and assess the captured tissue prior to applying electrocautery for tissue transection,” he said, noting that it should be completed “in a piecemeal fashion until the lesion is resected completely.”
Adjuvant techniques, such as hot avulsion or CAST (cold-forceps avulsion with adjuvant snare-tip soft coagulation), can be used to address small areas of residual tissue. Ideally, snare tip soft coagulation or argon plasma coagulation is applied to the resection margins.
100% Macroscopic Resection Rate
In the new study, Dr. Douglas along with senior author Matthew Moyer, MD, and their co-investigators, analyzed data from procedures done by three expert endoscopists at three different centers (abstract S130). They performed EMR-DC on 61 lesions that were 15 mm or larger that had been previously tattooed (n=1), biopsied (n=3), combination biopsied/tattooed (n=3) or subjected to a prior polypectomy attempt (n=54). The primary end point was complete macroscopic resection. Secondary end points were procedure time, recurrence at follow-up colonoscopy and adverse events.
The mean polyp size was 49 mm, and 84% were laterally spreading tumors. There was a wide distribution of Paris classification, most commonly IIa (44%), and a wide distribution of locations within the colon. Half of the patients (n=31) were on some form of anticoagulation.
For all of the 61 procedures, complete macroscopic resection was achieved. The recurrence rate at follow-up colonoscopy (mean time, 6.6 months) was 9.8%, which Dr. Douglas noted was more than acceptable “for these fairly complicated polyps.”
The mean procedure time was 49.5 minutes, with a range from 15 to 95 minutes. There were two serious adverse events: one post-polypectomy syndrome requiring intravenous antibiotics and hospitalization, and one case of post-polypectomy bleeding requiring a follow-up intervention.
In the discussion period, Dr. Douglas acknowledged that the study reflects the outcome with EMR-DC performed by “some of the best endoscopists in the world.” So, “there is the potential for bias,” he said, and more studies are needed to determine if these findings will be generalizable.
Importance of Preemptive Actions
Session co-moderator John R. Saltzman, MD, a professor of medicine at Harvard Medical School and the former director of endoscopy at Brigham and Women’s Hospital, both in Boston, commented that one of the take-home messages should pertain to what leads to this challenging scenario in the first place.
“We need to try to figure out what are the things that endoscopists do that lead to this, and to try to avoid those [actions],” he said. “One of the obvious things is tattooing. We need to tattoo away from the lesion. If anyone is still tattooing under the lesion, please do not do that.”
More generally, Dr. Saltzman emphasized, “If a procedure is beyond your comfort level of ability at the time, don’t do anything. Slow down. Do not partially do it.”
—Caroline Helwick
Drs. Douglas and Saltzman reported no relevant financial disclosures.
{RELATED-HORIZONTAL}