Colorectal neoplasms that are 4 cm or larger can be managed safely and effectively in the outpatient setting with endoscopic submucosal dissection, according to a patient series from Phillip S. Ge, MD, an assistant professor of medicine and advanced therapeutic endoscopist at The University of Texas MD Anderson Cancer Center, in Houston.
“Colorectal ESD can have a prominent role in the multidisciplinary management of large colorectal polyps (>4 cm) and offers the majority of patients an outpatient organ-sparing approach with excellent outcomes and low recurrence rates,” Dr. Ge said.
“Colorectal polyps less than 3 to 4 cm in size can often be managed with a high-quality EMR [endoscopic mucosal resection], with low risk for recurrence. However, ESD has an advantage and offers the ability to provide an en bloc resection when it comes to larger lesions, or those with fibrosis from prior polypectomy or tattooing that may be tricky to remove with EMR,” Dr. Ge explained.
Surgery for nonmalignant colorectal polyps is associated with significant morbidity and even mortality. The risk for a major postoperative adverse event is approximately 14%, with 3% to 4% of patients needing reoperation and 1% to 2% requiring colostomies (Clin Endosc 2018;87[1]:243-250); mortality risk is 0.7%, according to Dr. Ge.
“These are bad things we want to avoid, especially when ESD can offer comparable clinical outcomes in an outpatient setting,” he said.
‘Organ-Sparing’ Alternative To Surgery
George J. Chang, MD, MSc, a colorectal surgeon, a professor and the chair ad interim of the Department of Colon and Rectal Surgery at MD Anderson, who often collaborates with Dr. Ge, called ESD “a great organ-sparing solution for many patients” with adenomatous polyps that are large or associated with low-risk early cancer.
“Such polyps have to be removed completely and en bloc, and to do so often requires the special technical expertise of an advanced therapeutic endoscopist. … ESD can provide effective treatment without the need for major surgery,” he said.
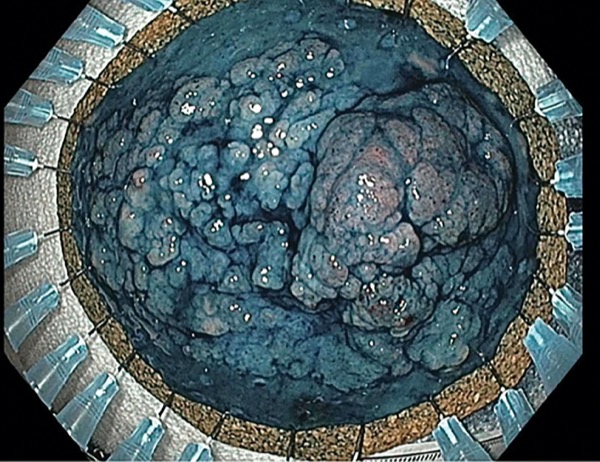
ESD, which can be performed throughout the gastrointestinal tract, was originally developed for the resection of early gastric cancer, Dr. Ge noted. In Western settings, ESD is increasingly being used for resection of large colorectal polyps, he said, yet the procedure is technically challenging and the learning curve for colorectal ESD steep. “It can be intimidating,” Dr. Ge acknowledged.
High Rates of Successful Resection
Dr. Ge, having accumulated enough data to study outcomes of ESD for large colorectal lesions, is fairly unique among advanced endoscopists. At the 2022 Digestive Disease Week (abstract 1448), he presented his findings on 127 patients with a combined total of 72 lesions in the right colon, 15 in the left colon and 40 in the rectum. Mean lesion size was 6.3 cm, and 30% were larger than 7 cm. Nearly one-third of the patients had been referred by a colorectal surgeon to undergo ESD as an organ-sparing alternative to surgical resection.
For 94% of the patients, ESD was performed in the outpatient setting; 6% required inpatient hospitalization, with a mean length of stay of 2.5 days. The mean resection time was 136 minutes, and mean resection speed was 13.6 cm2 per hour.
Adverse events were few and included delayed bleeding in three patients and rectal stricture in two patients, Dr. Ge reported. One patient experienced each of the following: a major intraprocedural bleed, microperforation, delayed perforation, urinary retention, transient bacteremia and pneumonia.
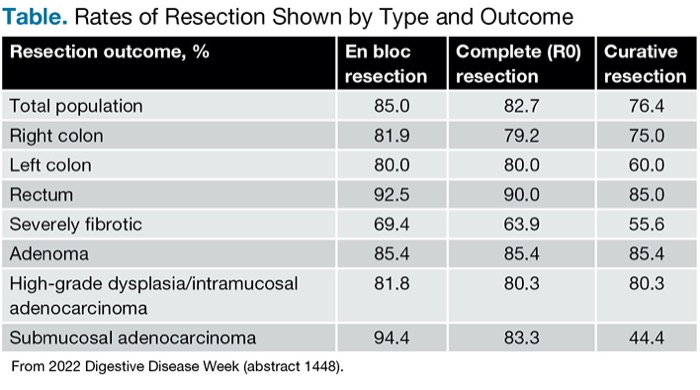
Rates of successful resection (en bloc, complete and curative) were high, and few patients required surgery (Table). “We can tell 76% of patients [are] cured of their disease,” Dr. Ge said.
| Table. Rates of Resection Shown by Type and Outcome | |||
| Resection outcome, % | En bloc resection | Complete (R0) resection | Curative resection |
|---|---|---|---|
| Total population | 85.0 | 82.7 | 76.4 |
| Right colon | 81.9 | 79.2 | 75.0 |
| Left colon | 80.0 | 80.0 | 60.0 |
| Rectum | 92.5 | 90.0 | 85.0 |
| Severely fibrotic | 69.4 | 63.9 | 55.6 |
| Adenoma | 85.4 | 85.4 | 85.4 |
| High-grade dysplasia/intramucosal adenocarcinoma | 81.8 | 80.3 | 80.3 |
| Submucosal adenocarcinoma | 94.4 | 83.3 | 44.4 |
| From 2022 Digestive Disease Week (abstract 1448). | |||
“Final pathology showed curative resection of tubulovillous adenoma with extensive high-grade dysplasia/intramucosal adenocarcinoma, with clear margins.”
Patients with less than curative resections can be sent for surgical consultations, “but few go forward with this,” Dr. Ge said. “For example, for a submucosally invasive, T1 colorectal cancer, the risk of lymph node metastases is less than 2%. Most patients in this situation consider this good enough and end up choosing surveillance rather than going forward with a radical surgical resection.”
Peter Draganov, MD, a professor of medicine at the University of Florida, in Gainesville, commented on the growing use of ESD for large colorectal lesions. “The results [of this study] reaffirm what has been published on the subject,” he said. “This study further supports that ESD for large colorectal lesions can be successfully and safely done in Western environments and now has become part of our armamentarium in the U.S.”
—Caroline Helwick
Dr. Chang reported a financial relationship with Medicaroid. Dr. Draganov reported financial relationships with Boston Scientific, Cook, Fujifilm, Medtronic and Olympus. Dr. Ge reported a financial relationship with Boston Scientific.
{RELATED-HORIZONTAL}