CHARLOTTE, N.C.—Clinically important serrated polyps are more likely to be detected on follow-up colonoscopy in patients who had a positive multi-target stool DNA test than in those who had a positive fecal immunochemical test or a colonoscopy without either test beforehand.
Patients with a positive multi-target stool DNA (mt-sDNA) test (Cologuard, Exact Sciences) were nearly three times as likely to be harboring clinically relevant serrated polyps (CRSPs) as those undergoing screening colonoscopy without the preceding stool-based test, and fecal immunochemical test (FIT)-positive patients were 1.5 times as likely, according to investigator Joseph C. Anderson, MD, a professor of medicine at Dartmouth Geisel School of Medicine, in Hanover, N.H.
“What these data suggest is that if you’re doing a colonoscopy on a patient who is mt-sDNA–positive, rather than just look for the large adenomas, you’ve got to be searching for serrated polyps, which is a different type of detection. You’ve got to have a high level of suspicion,” Dr. Anderson said.
He said the study addressed the common scenario of a positive finding on stool-based testing. Although the results likely reflect some differences in the tests’ sensitivity and specificity, the main point is that they reflect “clinically relevant” scenarios that are “more like everyday practice,” he said.
Dr. Anderson reported the findings in a poster at the 2022 annual meeting of the American College of Gastroenterology (abstract S251). The poster received a Presidential Poster Award.
Large Patient Database
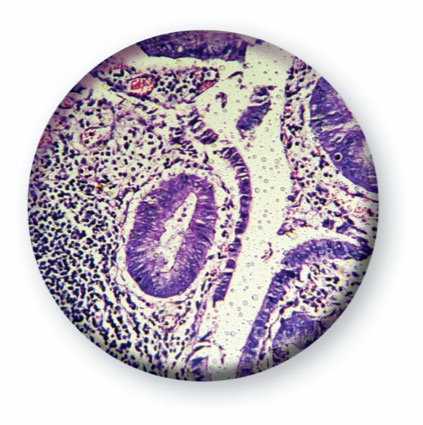
Patients in the study came from the New Hampshire Colonoscopy Registry (NHCR) and had received routine care between 2015 and 2020. The investigators compared those who had a colonoscopy after a positive mt-sDNA test (n=560) or after a positive FIT (n=414) with those who underwent screening colonoscopy alone (n=59,438) during the same period. The outcome of interest was CRSPs, which included all sessile serrated polyps, traditional serrated adenomas and hyperplastic polyps 1 cm or larger.
Polyp Findings After Positive DNA Test
When stratified by large adenomas, 18% of mt-sDNA–positive patients—or one in five—had CRSPs without synchronous large adenomas, compared with about 10% of FIT-positive patients (P<0.001) and 8% of colonoscopy-only patients (P<0.001). In the regression model, the odds ratio for detecting CRSPs was 2.86 for mt-sDNA and 1.2 for FIT, Dr. Anderson reported.
The researchers hypothesized that the mt-sDNA test would be more sensitive for CRSPs, which did not bleed, since it detects markers of methylation in addition to hemoglobin. “We wanted to look at those individuals who were not picked up because of bleeding,” Dr. Anderson said, noting that both the mt-sDNA test and FIT are good at detecting lesions that bleed.
The percentage of patients found to have large adenomas but no synchronous CRSPs was comparable between the stool-based methods: approximately 15% with mt-sDNA, 14% with FIT and 4% with colonoscopy only.
A Call for Careful Inspection
The findings support previous research in this area. “The results for Dr. Anderson’s study are not surprising, as they corroborate findings of the pivotal study comparing mt-sDNA and FIT with colonoscopy as the reference standard [N Engl J Med 2014;370(14):1287-1297],” commented Thomas Imperiale, MD, the Lawrence Lumeng Professor of Gastroenterology and Hepatology at Indiana University School of Medicine, in Indianapolis. “Endoscopists need to pay attention when results are consistent, as they are in this case,” Dr. Imperiale said.
“The clinical message is to be on the lookout for large sessile polyps, which may be challenging to find, particularly in the proximal colon,” he added. “Use of a cap or cuff should be considered.”
—Caroline Helwick
Dr. Anderson reported no relevant financial disclosures. Dr. Imperiale was the principal investigator for the pivotal study leading to the approval of Cologuard (Exact Sciences).
{RELATED-HORIZONTAL}