Endoscopic stricturotomy could be an alternative to endoscopic balloon dilation for managing some strictures related to inflammatory bowel disease. According to a study presented at the 2022 Crohn’s & Colitis Congress, ESt was successful in treating 90% of strictures in IBD patients, although roughly half of the patients required a repeat intervention within 18 months.
“While we need comparative efficacy and safety data, these findings provide good evidence that ESt is a useful tool for managing anastomotic and distal ileoanal strictures where, due to significant fibrosis, balloon dilation might not have durable efficacy and expandable stents may not be suitable,” commented Madhav Desai, MD, a gastroenterologist at Kansas City VA Medical Center, who was not involved in the study.
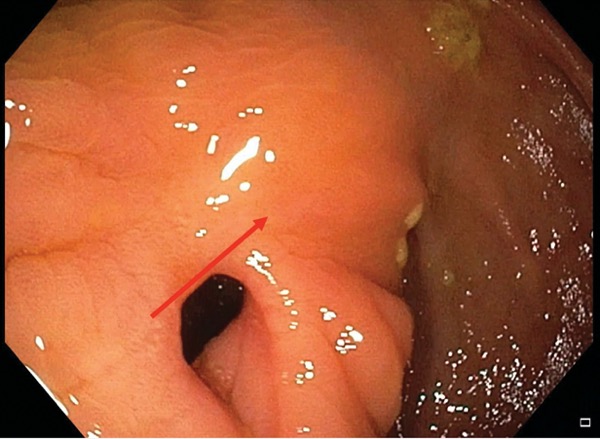
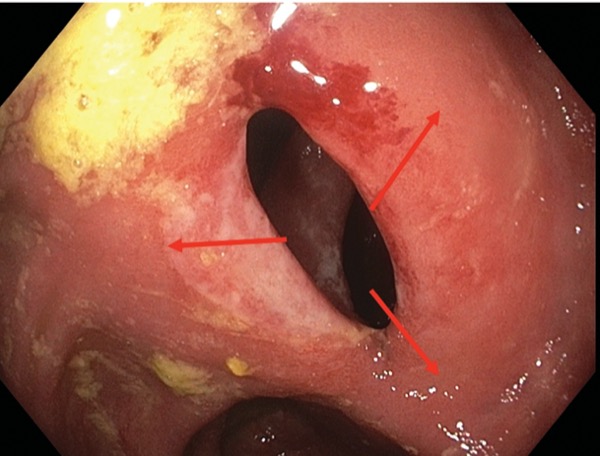
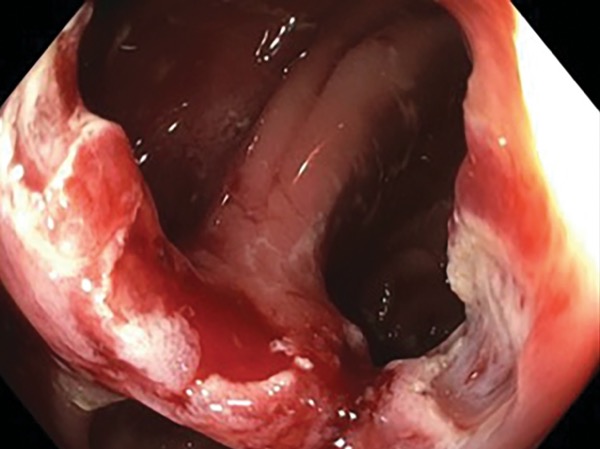
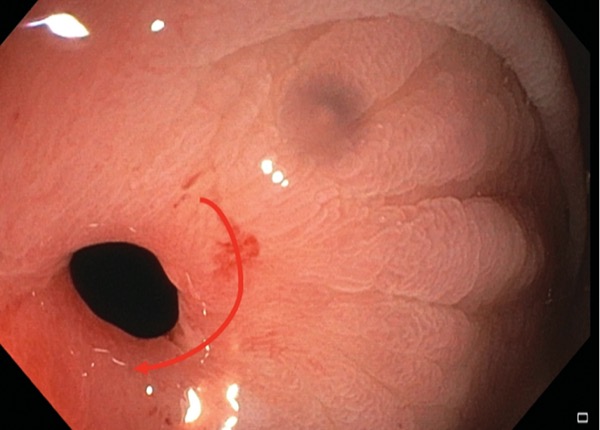
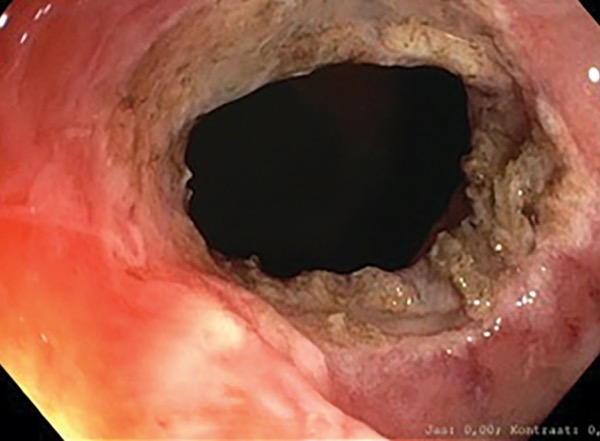
The procedure, pioneered at Cleveland Clinic, involves performing electroincisions in a stricture and removing fibrotic tissue. Clips can be used to prevent bleeding and space out incisions. Data from Cleveland Clinic published in 2017 indicated that “the rate of requirement for subsequent surgery after [endoscopic stricturotomy] with/without [endoscopic balloon dilation] seems to be lower than the historical rate of EBD reported in the literature” (Inflamm Bowel Dis 2017;2[4]:502-513).
{RELATED-VERTICAL}In the current study, lead researcher Martin Lukas, MD, a gastroenterologist at the IBD Clinical and Research Center at the ISCARE Clinical Center, in Prague, Czech Republic, and his co-investigators performed 92 stricturotomies in 67 patients, most of whom had Crohn’s disease. The patients were a mean age of 44 years and had IBD for a mean duration of 14.6 years. Over half of the procedures were preceded by at least one EBD and 27% by a stricturotomy, in the past.
Most of the strictures (89%) were anastomotic, including 64% located at an ileocolonic anastomosis, 10% at a colocolonic anastomosis, 12% at an ileal pouch–anal anastomosis and roughly 3% at an ileorectal anastomosis. The remaining strictures were new anal strictures.
According to Dr. Lukas, 90.2% of stricturotomies were technically successful, meaning the endoscope could be passed through the stricture immediately after the procedure. Four patients experienced delayed bleeding, which was managed conservatively, and there were no cases of perforation or other complications.
Follow-up data showed that 30.2% (95% CI, 15.6%-46.2%) of patients required another intervention, including ESt, EBD or surgery, at six months, 40.3% (95% CI, 25.5%-54.6%) required another intervention at one year, and 48.8% (95% CI, 34%-62.1%) needed another stricture intervention at 18 months. Dr. Lukas said a future publication will detail how many patients required surgery as a reintervention.
The time to reintervention was not related to the number and type of prior interventions, age of the anastomosis, patient age or sex, concurrent medications, or specific ESt technique employed, the investigators reported.
Approach Not Suitable for All Strictures
“We think there are two main factors determining the persistence of the effect of stricturotomy,” Dr. Lukas told Gastroenterology & Endoscopy News. “The first is that some strictures seem to be more refractory to treatment, whether stricturotomy or EBD. These strictures might have ongoing inflammation and fibrosis as well as a propensity for ischemia at the site of anastomosis.”
Another reason is that not all strictures are suitable for ESt, he said. Short and webbed strictures in which radial or horizontal incisions can be made are particularly amenable to ESt, Dr. Lukas explained (Figures 1-6). “Our preliminary results suggest that for strictures that are longer, softer and not mature enough for stricturotomy, balloon dilation is a more suitable approach.”
Dr. Desai commented that whereas ESt would require technical expertise and “knowledge of the nature of strictures, the learning curve does not seem like it would be very steep. When done in expert hands, ESt is a potentially efficient technique, and it could be particularly helpful in managing those patients who may not need surgery because they have otherwise quiescent disease, for example.” He added that ”the role and positioning of ESt for the management of IBD-related strictures will become clearer in the near future.”
—David Wild
The sources reported no relevant financial disclosures.