Performing a cold snare polypectomy isn’t easy—even after more than 100 procedures. That is the conclusion of a recent study that found fewer than 10% of trainees performed all steps competently after many attempts. For some steps, none of the GI fellows in the study reached competency, raising questions about the adequacy of fellowship programs in this area of practice.
“The learning curve for cold snare polypectomy [CSP] is long and varied among trainees, independent of video-based feedback,” said Tonya R. Kaltenbach, MD, a professor of clinical medicine at the University of California, San Francisco and the director of advanced endoscopy at the San Francisco VA Medical Center, who presented the findings at the 2021 virtual Digestive Disease Week (abstract 697). “Current apprentice-based training methods are not sufficient to allow trainees to achieve competency in CSP by the end of their fellowship.”
Aasma Shaukat, MD, a professor of medicine at the University of Minnesota, in Minneapolis, and an investigator with the U.S. Department of Veterans Affairs Center for Care Delivery and Outcomes Research, agreed.
“Complete polypectomy is a milestone for colonoscopy competency for trainees. However, we don’t know how well trainees can perform snare polypectomy or have evidence to support tools to improve their learning curve,” Dr. Shaukat said. “This study reports that most trainees do not achieve CSP with the current apprentice-based training model, and that there is likely a role for video-based training and feedback in addition, in order to improve these skills.”
CSP: A Staple of Endoscopy
Cold snare polypectomy is the recommended technique for the removal of small polyps (under 1 cm)—which account for more than 75% of all polyps—but has been associated with significant variability in competency and teaching among attendings. The learning curve for CSP, and the impact of video feedback on trainee competence, are unknown, Dr. Kaltenbach said.
Her multicenter, randomized, single-blind trial aimed to determine the variability of competency in CSP of small lesions among trainees, and to compare performance over time between trainees who received video-based feedback and those who received conventional apprentice-based feedback. “We hypothesized that video feedback would accelerate competence,” Dr. Kaltenbach said.
The study randomized 22 trainees, 12 to video feedback and 10 to conventional feedback, who performed a total of 2,339 colonoscopies. The two groups performed a similar number of colonoscopies and polypectomies, but the video feedback group resected more sessile polyps (1,285 vs. 901; P=0.027).
Expert, blinded raters evaluated 12 deconstructed CSP steps and the overall performance of CSP using the validated four-point cold snare polypectomy assessment tool (CSPAT). The CSPAT rating scale is 1 for “unacceptable,” 2 for “suboptimal,” 3 for “adequate and 4 for “perfect.”
The primary outcome was the number of trainees who achieved competency (CSPAT 3-4) across all domains.
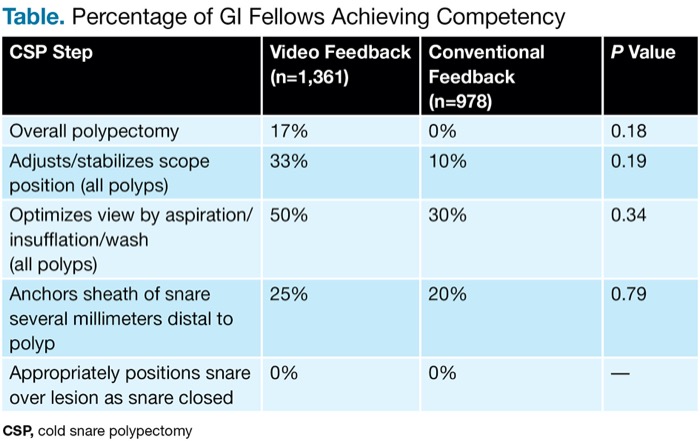
Two of 22 trainees achieved competency by the end of the training period. For these two clinicians, who were both in the group that received video feedback, the mean CSP volume to gain competency was 135 polypectomies, Dr. Kaltenbach reported (Table).
| Table. Percentage of GI Fellows Achieving Competency CSP, cold snare polypectomy | |||
| CSP Step | Video Feedback (n=1,361) | Conventional Feedback (n=978) | P Value |
|---|---|---|---|
| Overall polypectomy | 17% | 0% | 0.18 |
| Adjusts/stabilizes scope position (all polyps) | 33% | 10% | 0.19 |
| Optimizes view by aspiration/insufflation/wash (all polyps) | 50% | 30% | 0.34 |
| Anchors sheath of snare several millimeters distal to polyp | 25% | 20% | 0.79 |
| Appropriately positions snare over lesion as snare closed | 0% | 0% | — |
Trainee competency increased by 3% after every 20 CSPs in the video feedback group, while no incremental improvements were observed with the apprentice-based feedback (P=0.0004), Dr. Kaltenbach said.
A Fellow’s Thoughts
The findings highlight fundamental challenges in endoscopic training during fellowship, according to Muddasir Ayaz, MD, a GI fellow at the University of Buffalo, in New York. “They upend the idea that competency can be achieved by simply reaching a number,” he said. “Many endoscopists would have assumed that performing over 100 cold snare polypectomies would lead to competency, and Dr. Kaltenbach and her colleagues clearly demonstrate the limitations of such assumptions. Overall, the study highlights unique opportunities for introspection for many program directors and offers useful adjuncts to the current training paradigm for cold snare polypectomy.”
Dr. Ayaz added that the findings “argue against the long-standing belief that endoscopic skills are translatable.” He noted that most educators in endoscopy “believe and teach the notion that achieving competency in one arena of endoscopy will lead to gains in other arenas.”
While the study does not specifically address this issue, he said, “it does highlight that certain skills require specific, intensive feedback to achieve competency, and creates further opportunities for investigation of other endoscopic skills that warrant unique pedagogical approaches.”
Dr. Ayaz also said the findings may not be generalizable to other fellowship programs.
In this study, half the fellows received intensive feedback that “likely exceeds what is offered in most programs,” he said. “It is also unclear if the targets outlined in the study represent aspirational goals during fellowship, given the competing priorities of achieving competency with other endoscopic skills during GI fellowship. Some discussion regarding whether their targets represent mastery rather than competency is worth exploring as well.”
—Caroline Helwick
Drs. Ayaz, Kaltenbach and Shaukat reported no relevant financial disclosures.