Division of Gastroenterology and Hepatology at the University of North Carolina at Chapel Hill School of Medicine

Division of Gastroenterology and Hepatology at the University of North Carolina at Chapel Hill School of Medicine

In this installment of “Expert Picks,” assistant professor Shifali Arora, MD, and associate professor Anne Peery, MD, both in the Division of Gastroenterology and Hepatology at the University of North Carolina at Chapel Hill School of Medicine, highlight important research related to COVID-19 presented at the 2021 virtual Digestive Disease Week.
Abstract 436. Increased Burden of Alcohol-related Gastrointestinal And Liver Diseases During the COVID-19 Pandemic: A Hospital System Wide Audit (Chung et al)
In this study, researchers conducted an audit of all inpatient gastrointestinal consults performed at Rhode Island Hospital during the COVID-19 lockdown phase (March 23 to May 10, 2020) and the reopening phase (June 1, 2020) and compared the data against data from 2019 to identify any fluctuations in disease burdens. The researchers identified 558 consults during the lockdown phase and 713 during the reopening phase.
The volume of inpatient consults decreased sharply at the onset of the pandemic but quickly returned to normal levels during the reopening phase. During the lockdown phase, overall consults decreased by 27.7% compared to the same time period in 2019. However, but the proportion for alcohol-related GI and liver diseases—including alcoholic hepatitis, alcoholic cirrhosis, alcoholic pancreatitis and alcoholic gastritis—increased by roughly 60% (P=0.03). During the reopening phase, the proportion of consults for alcohol-related GI and liver diseases remained elevated by 78.7% (P=0.01), and consults for alcoholic hepatitis were increased by 127.2% (P<0.01). Also increased was the percentage of people with alcohol-related GI and liver disease requiring inpatient endoscopic interventions (34.6% vs. 13.8%; P=0.04), the researchers reported.
Dr. Peery: Before the COVID-19 pandemic, alcohol-associated liver disease incidence and mortality was increasing. Chung et al found an increased burden of alcohol-related inpatient consults during the pandemic. The increase may have resulted from delays in or limited access to health care. It is also possible that alcohol consumption increased during the pandemic. This is an important reminder to follow the United States Preventive Task Force recommendation to screen all adult patients for unhealthy alcohol use and when appropriate to provide brief behavioral counseling as well as resources.
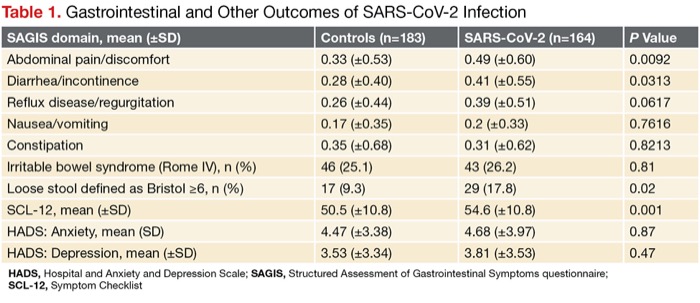
Abstract 782. Persistent Gastrointestinal Symptoms and Chronic Fatigue After SARS-COV-2 Infection (Noviella et al)
In this study, researchers in Italy investigated the prevalence of GI symptoms and chronic fatigue by means of a structured questionnaire after the resolution of SARS-CoV-2 infection and compared the results to individuals without the virus. There were 164 patients with SARS-CoV-2 (mean age, 44 years; 40% women) and 183 control subjects without the novel coronavirus (mean age, 40 years; 61% women). The researchers found that fever, shortness of breath, loss of smell and taste, fatigue, muscle pain, diarrhea, weight loss and antibiotic treatment were more frequent in patients during the infection. After the infection resolved, the severity of abdominal pain/discomfort, diarrhea/incontinence symptoms and loose stools (Table) was more common in people with SARS-CoV-2 than in controls, as was the share of people with chronic fatigue chronic fatigue (31.7% vs. 13.7%, respectively; P<0.001). The results suggest that SARS-CoV-2 may affect the brain–gut axis in the long term, according to the investigators.
| Table 1. Gastrointestinal and Other Outcomes of SARS-CoV-2 Infection | |||
| SAGIS domain, mean (±SD) | Controls (n=183) | SARS-CoV-2 (n=164) | P Value |
|---|---|---|---|
| Abdominal pain/discomfort | 0.33 (±0.53) | 0.49 (±0.60) | 0.0092 |
| Diarrhea/incontinence | 0.28 (±0.40) | 0.41 (±0.55) | 0.0313 |
| Reflux disease/regurgitation | 0.26 (±0.44) | 0.39 (±0.51) | 0.0617 |
| Nausea/vomiting | 0.17 (±0.35) | 0.2 (±0.33) | 0.7616 |
| Constipation | 0.35 (±0.68) | 0.31 (±0.62) | 0.8213 |
| Irritable bowel syndrome (Rome IV), n (%) | 46 (25.1) | 43 (26.2) | 0.81 |
| Loose stool defined as Bristol =6, n (%) | 17 (9.3) | 29 (17.8) | 0.02 |
| SCL-12, mean (±SD) | 50.5 (±10.8) | 54.6 (±10.8) | 0.001 |
| HADS: Anxiety, mean (SD) | 4.47 (±3.38) | 4.68 (±3.97) | 0.87 |
| HADS: Depression, mean (±SD) | 3.53 (±3.34) | 3.81 (±3.53) | 0.47 |
| HADS, Hospital and Anxiety and Depression Scale; SAGIS, Structured Assessment of Gastrointestinal Symptoms questionnaire; SCL-12, Symptom Checklist | |||
Dr. Arora: Post-infectious irritable bowel syndrome is a well-accepted and treatable phenomenon. The work by Noviella et al found that patients who have had COVID-19 are at increased risk for ongoing GI symptoms. We will likely see these patients in our clinics. Using what we know about post-infectious IBS, we should give these patients a definitive diagnosis, provide education on the brain–gut axis, and when necessary, treat predominant symptoms.
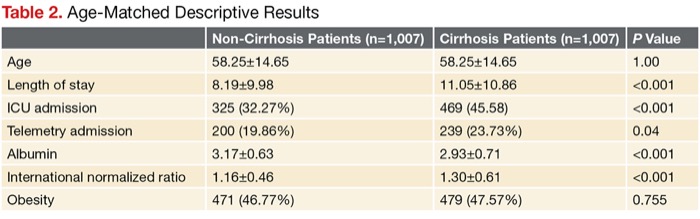
Abstract 6. Cirrhosis Is Associated With Significantly Worsened Clinical Outcomes of COVID-19 Infection in a Retrospective Analysis of 23,474 Patients Across 143 Hospitals (Hwang et al)
This study showed that patients with both cirrhosis and COVID-19 experienced significantly worse outcomes than patients with COVID-19 alone. The findings come from an analysis of data from the HCA Healthcare Physician Services clinical data warehouse that involved 23,470 adults across admitted to a group of 143 hospitals from January to August 2020 with COVID-19. Of those, 1,007 COVID-19 patients had cirrhosis and 22,467 COVID-19 patients did not have the liver disorder.
Patients with both COVID-19 and cirrhosis had higher mortality (17.97% vs. 12.96%; P<0.001), higher rates of ventilation (24.% vs. 16.07%; P<0.001) and longer lengths of stay in the hospital (11.05 vs. 8.46 days; P<0.001), according to the researchers. The outcomes of ICU admission and length of stay remained significant on paired t test when the 1,007 patients with COVID-19 and cirrhosis were age-matched to COVID-19 patients without cirrhosis. On multivariable analysis, cirrhosis was independently associated with increased mortality (odds ratio [OR], 1.33; P=0.002), ICU admission (OR, 2.08; P<0.001) and ventilation (OR, 1.32; P<0.001). Similar to previous studies, the data suggested protective effects of female sex and deleterious effects of increasing age, myocardial infarction, cerebrovascular disease, diabetes, cancer and obesity.
| Table 2. Age-Matched Descriptive Results | |||
| Non-Cirrhosis Patients (n=1,007) | Cirrhosis Patients (n=1,007) | P Value | |
|---|---|---|---|
| Age | 58.25±14.65 | 58.25±14.65 | 1.00 |
| Length of stay | 8.19±9.98 | 11.05±10.86 | <0.001 |
| ICU admission | 325 (32.27%) | 469 (45.58) | <0.001 |
| Telemetry admission | 200 (19.86%) | 239 (23.73%) | 0.04 |
| Albumin | 3.17±0.63 | 2.93±0.71 | <0.001 |
| International normalized ratio | 1.16±0.46 | 1.30±0.61 | <0.001 |
| Obesity | 471 (46.77%) | 479 (47.57%) | 0.755 |
Dr. Peery: Despite wide availability, only 40% of the U.S. population is now fully vaccinated against SARS-CoV-2. The work by Hwang et al highlights how this patient population can be affected if they were to have COVID-19. It is an important reminder to make time to educate patients with cirrhosis to get a COVID-19 vaccine. This work and other studies have found that patients with cirrhosis are at increased risk for poor outcomes from COVID-19. Vaccination may reduce these risks and should be encouraged.
Abstract 337. Comparing Patient Satisfaction Among Telemedicine, Direct Access, and In-Person Clinic Pre-Procedure Visits for Gastrointestinal Advanced Endoscopic Procedures (Wee et al)
This study compared patient satisfaction in individuals who had preprocedure consultation visits by telemedicine, in–person or a direct access procedure (instructions and procedure explained by a nurse practitioner or physician assistant). The study included patients who had undergone an advanced endoscopic procedure at Long Island Jewish Medical Center, in Queens, N.Y., between May and August 2020.
Over the telephone, patients completed a modified version of the modified Group Health Association of America-9, which evaluated satisfaction with pre-procedure, intra-procedure and post-procedure experiences. Researchers grouped patients based on whether they had received an in-clinic consultation visit by the endoscopist, a telemedicine consultation visit by the endoscopist or direct access. The researchers gathered information regarding geographic location to the office, prior endoscopic experience, type of endoscopic procedure (diagnostic vs. therapeutic) and a new diagnosis of GI cancer.
Of the 322 patients called, 123 provided responses to the survey. Of those, 26 patients had an in-person consultation, 32 had a telemedicine consultation, and 65 had a direct access consult. Overall mean satisfaction among the three groups did not differ significantly (P=0.983). In addition, subanalysis of the pre-, intra- and post-procedure satisfaction scores did not reveal statistically significant differences (P=0.996, P=0.244 and P=0.998, respectively). Among people with a new diagnosis of GI cancer, those who had telemedicine visits with proceduralists had a statistically significant higher mean satisfaction score than those who had direct access procedures (P=0.0116), according to the researchers.
Dr. Arora: Prior to the COVID-19 pandemic, use of telemedicine in gastroenterology was minimal. As many of us had to abruptly stop in-person visits, telemedicine provided a way to reach our patients and continue to provide care. The work by Wee et al highlights that patient satisfaction is similar using this modality and may be an option even as we start to reopen our clinics. It may provide us with an additional tool to help patients who live farther away or have limited transportation options.
—Compiled and written by Kate O’Rourke