Bedside ultrasound can facilitate efficient and meaningful changes in the management of patients with inflammatory bowel disease.
Among other things, a study found that use of bedside intestinal ultrasound obviated the need for ER visits, in-hospital endoscopy and hospitalization—benefits felt even more acutely during the COVID-19 pandemic.
“I was exposed to intestinal ultrasound through a radiologist who primarily focused on the GI tract and liver,” said Kerri L. Novak, MD, a clinical associate professor of medicine at the University of Calgary, in Alberta. “After spending some time with her, I began to realize that gastroenterologists can do this themselves.”
When the pandemic started, Dr. Novak and her colleagues recognized how access to routine endoscopy would plummet and how they also needed to keep patients out of the emergency department and hospital. “We created a centralized model where we provide ultrasound as a tool to objectively and accurately measure what’s going on with IBD patients,” she said.
As part of the investigation, the researchers prospectively evaluated the impact of the care pathway among a group of 72 established IBD patients (57% women; 65.5% with Crohn’s disease) with symptoms suggestive of a disease flare, or those at high risk for a new IBD diagnosis. All patients were seen in the institution’s urgent access clinic between March 15 and June 30, 2020.
As Dr. Novak reported during Canadian Digestive Diseases Week 2021 (abstract A173), all patients were seen within seven days of referral. In total, 84.7% (61/72) of patients underwent a substantial management change based on features of active inflammation detected by either intestinal ultrasound alone (53%; 38/72), sigmoidoscopy alone (12.5%; 9/72) or a combination of the two methods (32%; 23/72).
Five patients (8.2%) required biologic dose escalation, 12 (19.7%) underwent either the introduction of a biologic or a biologic class switch, and eight (13%) required topical or systemic corticosteroids.
Six patients were referred to colorectal surgery for resection of complicated disease first characterized by intestinal ultrasound, including two emergent procedures. Clinicians made three new diagnoses of IBD: one case of colonic Crohn’s disease and two of ulcerative colitis.
No patients visited the emergency department during the study period, and acute care in-hospital endoscopy was avoided in 80.6% (58/72), according to the researchers. Eight patients were scheduled for subsequent elective, nonurgent colonoscopy, either for the suspicion or absence of disease requiring routine confirmation.
Despite the benefits, Dr. Novak noted that ultrasound can be technically challenging, and requires specialty training. The International Bowel Ultrasound Group (ibus-group.org), a nonprofit group based in Germany, has established a four-week training program for clinicians interested in becoming credentialed in the procedure, she added.
“I would push gastroenterologists to recognize the importance of patient preference with respect to our ability to make timely decisions in clinic,” Dr. Novak said. “We need to invest in new ways of looking at the bowel, and this is one of them.”
Michael Stewart, MD, an assistant professor of medicine at Dalhousie University in Halifax, Nova Scotia, said bedside intestinal ultrasound offers a perspective on IBD that few other imaging modalities can match.
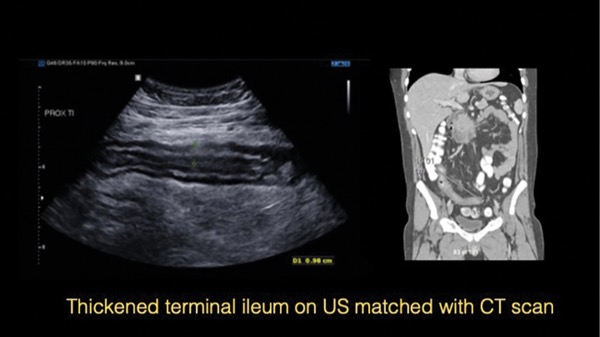
“It gives us a bit more of a functional understanding of what’s happening in the bowel,” Dr. Stewart said. “For example, if a patient has a narrowing or stricture in their bowel, a CT scan might show some thickening of the bowel in that location, but it may not show anything else. Because ultrasound is a dynamic study, it’s like watching a movie rather than looking at still photographs. So, if the bowel is contracting, you can see whether the stricture is having a functional impact.”
But Dr. Stewart noted that certain parts of the bowel are not particularly well imaged with ultrasound. “The rectum and the proximal small bowel can be very hard to image,” he said. “All the tools we have access to have their particular benefits and drawbacks, and are all useful in various contexts.”
—Michael Vlessides
Drs. Novak and Stewart reported no relevant financial disclosures.