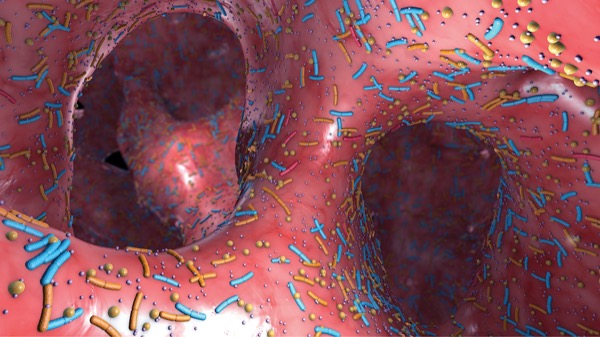
A sophisticated characterization of the small-bowel microbiome could aid the search for treatments for small intestinal bacterial overgrowth (SIBO). Compared with controls, Klebsiella and Escherichia dominated the altered microbiome of SIBO patients and might be targets for restoring a healthier microbial balance, researchers have found.
The SIBO analysis was drawn from the ongoing REIMAGINE study, which is using several emerging techniques to sample and sequence the microbiome. Computational strategies applied to characterize microbial interrelationships are proving to be a “powerful approach to generate meaningful insights in complex biological systems,” said Leopoldo Valiente-Banuet, a researcher with the Medically Associated Science and Technology (MAST) program at Cedars-Sinai Medical Center, in Los Angeles, who contributed to the study.
Mr. Valiente-Banuet and his colleagues analyzed microbiome samples from 34 people with SIBO and 34 volunteers without the condition. Klebsiella and Escherichia were identified as “the most important disrupters of the integrity of the microbiome network,” said Mr. Valiente-Banuet, who performed the work in collaboration with senior author Mark Pimental, MD, the executive director of the MAST program.
The effects are systemic and “are further exemplified by dramatically reduced connectivity at the genus level,” Mr. Valiente-Banuet reported. He noted that the density of triangle motifs, which describes one approach to tracing relationships in complex networks, was severely reduced in SIBO versus non-SIBO microbiomes, a change likely related to increased growth of Escherichia (P=0.011) and Klebsiella (P<0.001). The alterations in taxa were seen at different levels among all phyla.
The importance of the microbiome to the health and function of the gastrointestinal tract and other biological systems is well recognized. Although there has been progress in characterizing differences between a healthy microbiome and the microbiome signatures of several disease states, the complexity remains daunting, according to an overview of the challenges (Clin Gastroenterol Hepatol 2019;17[2]:218-230). It’s difficult to confirm whether any change in the microbiome is causative rather than just associated with a given disease.
The network analysis used in this study is promising for the larger effort to trace the pathogenicity of microbial alterations, according to Mr. Valiente-Banuet. He said the data provide a basis for studying the impact of the small-bowel microbiome on SIBO and a path for understanding the imbalances that drive this disease and for considering treatments. The same approach is likely applicable to interventions for other diseases linked to microbiome deviations.
Although the area of research is promising, translating it into new treatment strategies requires overcoming several obstacles, according to Purna S. Kashyap, MBBS, the co-director of the microbiome program at the Center for Individualized Medicine at Mayo Clinic College of Medicine and Science, in Rochester, Minn.
“We do think that the small intestinal microbial composition is likely to be as or a more important determinant of symptoms than overgrowth of bacteria alone, but we still need to demonstrate the relationship between specific microbial members and GI symptoms before we can embark on a therapeutic strategy,” Dr. Kashyap said.
He offered a cautionary note about the use of MacConkey agar for the culture medium. This medium is selective for gram-negative bacteria, so the strong representation of Klebsiella and Escherichia in SIBO-positive patients was “not surprising,” but he agreed that network analysis is an appropriate first step to document the relationship between microbes.
“Such network analyses are important and would be even more relevant when combined with clinical data,” he said, referring to the need to show a correlation between overgrowth of specific bacteria and SIBO-related symptoms.
—Ted Bosworth
Mr. Valiente-Banuet and Dr. Kashyap reported no relevant financial disclosures. Mr. Valiente-Banuet presented the findings at the 2020 virtual meeting of the American College of Gastroenterology (abstract P2631).