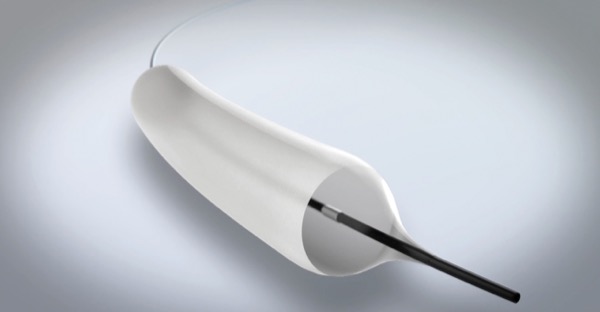
A balloon coated with the anticancer agent paclitaxel appears to hold significant promise for the treatment of patients with complicated esophageal stents.
One year after dilatation with the experimental therapy, from GIE Medical, eight of nine patients with benign strictures have yet to experience a recurrence, researchers have found. Although the data are preliminary, experts said the findings, reported at the 2021 Digestive Disease Week (abstract 818), could herald a major advance in the management of esophageal narrowing.
“The long-term control in this series of complex strictures was achieved after a single intervention,” reported study leader Kenneth K. Wang, MD, the Russ and Kathy Van Cleve Professor of Gastroenterology Research and director of the Barrett’s esophagus unit at Mayo Clinic in Rochester, Minn.
Although it was a pilot study, the consistency of the outcomes at 12 months has already provided the basis for a randomized trial for which Dr. Wang is recruiting participating centers.
“Benign recalcitrant esophageal strictures are difficult to manage endoscopically, as they do not respond well to endoscopic treatment like conventional esophageal dilations, stents, stricturoplasty, steroids or mitomycin C injection, which leads to recurrent strictures causing severe dysphagia,” said Shreyas Saligram, MD, an assistant clinical professor of gastroenterology at UT Health San Antonio. “Therefore, there is a need for an alternative treatment that can effectively dilate the benign recalcitrant esophageal strictures, which can give durable resolution of symptoms.”
Paclitaxel-coated balloons have been widely used for the treatment of stenotic vascular lesions for more than 20 years. The mechanism of benefit in the esophagus is believed to result from the same antiproliferative and antifibrotic effects that prevent arterial restenosis, Dr. Wang said.
For the new study, Dr. Wang’s group recruited 10 patients, of whom one was excluded when malignancy was detected. Prior to the study, patients had a mean of two conventional dilatations. The mean diameter of the esophagus before treatment with the paclitaxel-coated balloon was 6 mm.
“These were patients with bad complex strictures. The average length was 6.4 mm,” Dr. Wang said.
The paclitaxel-coated balloons are available in three sizes. The smallest has an inflation range of 8 to 12 mm, the midsize balloon has a range of 12 to 15 mm, and the largest ranges from 18 to 20 mm. Most patients were treated with the balloon that had a maximum 15-mm inflation. In the protocol, the inflation, which is performed under anesthesia, is maintained for five minutes.
“The usual time for a conventional balloon dilation is about one minute, but the inflation time is longer with the drug-coated stent to allow the drug to disseminate,” Dr. Wang explained.
Upper GI imaging was performed before and three months after inflation to obtain precise measurements of the procedure’s effect. At three months, the mean diameter of the esophagus, at 13.6 mm, represented a more than doubling from baseline.
No adverse events were associated with the procedure or side effects from exposure to the paclitaxel, Dr. Wang said.
“The drug exposure is fairly low. Even with maximum five-minute dilation with the 20-mm balloon, patients only receive about 11 mg of paclitaxel,” he said.
It’s too soon to determine whether a subset of patients will be free permanently of recurrence after a single treatment, according to the researchers, but the lack of recurrence in all but one patient in this series of refractory strictures was promising.
In the pivotal controlled trial, patients will be randomized to the drug-coated balloon or a conventional balloon. The primary outcome will be time to recurrence, Dr. Wang said.
Multiple Applications Envisioned
The most likely indication for the paclitaxel-coated balloon is for treatment of patients with refractory stricture, according to Dr. Wang, who added that the device could be a significant advance in other ways. One potential indication, he said, would be for treating complications of endoscopic mucosal resection (EMR).
“For EMR, one of our biggest problems is stricture. These can be nasty and resistant to treatment. If we had a better therapy for stricture, it would obviate the need for the more conservative resection we now perform to reduce the risk of stricture. This could be incredibly important for reducing cancer recurrence,” Dr. Wang said.
New strategies for treating refractory benign esophageal strictures are welcome, according to Kulwinder S. Dua, MD, a professor of medicine and pediatrics at the Medical College of Wisconsin, in Milwaukee.
“The major limitation of this study is that only nine patients were studied, of which six had peptic strictures and one had eosinophilic esophagitis. Strictures from both of these causes are easier to manage with conventional approaches and medications than complex strictures caused by radiation, corrosives, mucosal resections and surgery,” Dr. Dua noted.
He acknowledged that the data are “promising,” but said he awaits larger and more rigorous studies. “Prospective, randomized controlled trials are required, including patients with strictures from other causes besides strictures related to peptic causes of EoE,” he said.
—Ted Bosworth
Dr. Dua reported financial relationships with Boston Scientific, Cook Medical and Merit Medical. Dr. Wang reported financial relationships with Boston Scientific and Olympus.