Adherence to published surveillance guidelines for esophageal varices in patients with cirrhosis can be bolstered by the introduction of an automated prescriptive template, researchers have found.
“We noticed there was quite a bit of variability between different endoscopists in their reporting conventions following endoscopy for varices surveillance in patients with decompensated cirrhosis,” said Danielle Brandman, MD, an associate professor of clinical medicine at the University of California, San Francisco. “And we saw this as a very simple place for intervention. Because if we as gastroenterologists and hepatologists are not providing the correct recommendations, how can we expect anyone reading the report to do the right thing?”
To address this issue, Brandman and her colleagues initiated a quality improvement project aimed at improving adherence among clinicians when documenting management recommendations for patients with esophageal varices. The template utilized a standardized set of follow-up recommendations, which were derived from best practices published by the American Association for the Study of Liver Diseases and the American Society for Gastrointestinal Endoscopy.
“Once we decided on the appropriate follow-up recommendations after endoscopy, we worked with our IT staff for the endoscopic reporting program to construct an appropriate template,” Brandman told Gastroenterology & Endoscopy News. The template was incorporated into the Pentax endoPRO system as part of the institution’s standardized procedural documentation, offering preselected follow-up and treatment recommendations.
A subsequent educational campaign was designed to inform clinicians of the changes and introduce them to the new template. “We sent emails to everyone performing endoscopies, both at the fellow and faculty level,” Brandman said. “We also posted flyers in the endoscopy unit, right above the workstations where providers complete their reports.”
In a presentation at the 2020 digital Liver Meeting (abstract 631), Brandman’s group compared results among inpatients and outpatients with cirrhosis who had esophageal varices on esophagogastroduodenoscopy (EGD) at her institution between January 2018 and March 2020.
In total, 2,363 EGDs were performed during the pre-intervention period (January 2018-May 2019). Esophageal varices were evident in 218 of these procedures, 54% of which did not have adequate documentation of the size of the lesions. Of the 127 EGDs with documented esophageal varices size and/or endoscopic variceal ligation, only 63% provided appropriate guideline-based follow-up recommendations, according to the researchers.
A survey performed at the time revealed that suboptimal adherence in documenting surveillance recommendations was largely the product of variability in provider practices, as well as a low satisfaction rate with the existing endoscopy template among clinicians.
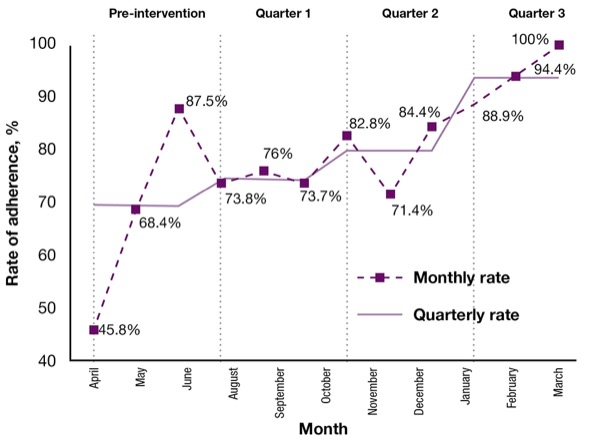
In the period following implementation of the automated endoscopy template (June 2019-March 2020), 223 EGDs were performed. Over that nine-month period, adherence in documenting guideline recommendations rose steadily in each quarter, from 69% in the pre-intervention period to 74% (64/86 EGDs), 80% (71/89 EGDs) and 94% (45/48 EGDs), the researchers reported (Figure). The primary reason clinicians failed to appropriately document management recommendations was because providers failed to use the updated template.
Brandman said the results exceeded her group’s expectations. “We’re very proud of this very simple intervention, which has the potential to lead to improved quality of care,” she said.
Equally surprising was the fact that there was little pushback from clinicians. “I think a lot of times people can become set in their ways, and we were asking them to change their behavior,” she said. “But I think we made it as easy as possible for them. And non-hepatologist gastroenterologists recognized that these are patients they don’t take care of very frequently, so they welcomed any assistance we offered.”
Richard S. Zubarik, MD, a professor of gastroenterology at the University of Vermont Medical Center, in Burlington, credited the utility of the UCSF approach. “I think having templates that are geared towards specific clinical scenarios, such as esophageal varices band ligation, can help ensure that guidelines are followed.”
Adherence is particularly difficult given the range of society recommendations that may exist. “Guidelines also vary according to the clinical situation,” Zubarik said. “I don’t think many physicians have a great handle on when to recommend subsequent procedures. But by using a template such as this, they’re more likely to comply with societal recommendations, and that’s a good step.”
Still, Zubarik expressed some doubt about whether the improved adherence observed in the study can actually translate to improved patient care: “There’s also the question of whether the findings from short-term quality improvement studies can be sustained, and whether the results are generalizable to other centers.”
—Michael Vlessides
Brandman and Zubarik reported no relevant financial disclosures.