This month, I’ve chosen three studies that highlight how we can optimize the diagnosis and management of eosinophilic esophagitis (EoE). The first study emphasizes the importance of careful examination and systematic biopsy akin to Barrett’s esophagus. It suggests a new protocol for sampling and obtaining an adequate number of biopsies in EoE. Current guidelines state that we should obtain at least six biopsies from the distal and proximal esophagus in patients with suspected EoE.
The second study describes a high prevalence of EoE in first-degree relatives (FDRs) of patients with this condition, particularly when these relatives have allergy symptoms. The results highlight the importance of obtaining a good family and personal history from patients with EoE, and they encourage family members with symptoms of allergies to discuss diagnostic considerations of EoE with their providers. The findings also point to the need to explore genetic associations in the pathogenesis of this condition.
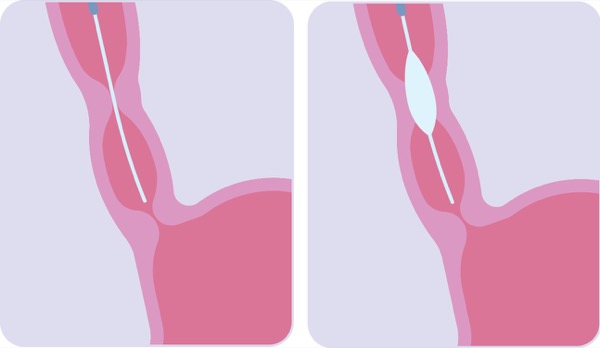
The last study looked at the use of esophageal dilation alone as a long-term treatment for difficult-to-treat EoE. Right now, fewer than 20% to 30% of patients are treated with dilation alone, but these results demonstrate the therapy can be considered a long-term strategy with fair success and minimal complications. This salvage option in patients who are otherwise nonresponsive to other therapies will need to be studied in prospective trials to more fully delineate its risks and benefits.
In Denmark, Adequate Number Of Biopsies Increase EoE Diagnoses 50-Fold (Endoscopy 2021;53[1]:15-24)
After finding very few cases of EoE diagnosed in the North Denmark Region between 1999 and 2010, experts there developed a consensus biopsy protocol to ensure appropriate diagnosis of the condition in patients with dysphagia. The protocol recommends that four biopsies be taken at 4 and 14 cm above the esophagogastric junction in these patients—the so-called 4-14-4 rule—and encourages clinicians to consider a diagnosis of EoE if histology reveals 15 or more eosinophils per high-power field.
The impact of the new protocol has been profound, as the researchers report. The number of patients diagnosed with EoE increased from a median of one per year between 2007 and 2011 to a median of 52 annually after the protocol was implemented (P<0.001). During the same period, clinicians doubled the number of biopsies obtained per patient, from a median of four in 2007 to a median of eight in 2017 (P<0.04).
Don’t Forget FDRs of EoE Patients (Clin Gastroenterol Hepatol 2020 Nov 18. [Epub ahead of print])
Researchers in Salt Lake City enrolled 239 adult FDRs of 37 patients with EoE. They examined their medical records; administered questionnaires about reflux, dysphagia, and allergy and atopy symptoms; and performed endoscopies in 71 patients.
Roughly 15% of all FDRs had EoE, found either through endoscopic examination or medical record analysis. Hay fever, allergic eye symptoms and reported food allergy symptoms were significantly more common in FDRs with EoE, compared with those without. Allergic rhinitis and asthma were not associated with a higher likelihood of EoE. Other significant risk factors for EoE in FDRs included male sex, younger age and higher serum eosinophils.
Esophageal Dilation as Stand-Alone Long-Term Treatment (American College Of Gastroenterology 2020 annual meeting; poster 0834)
Researchers at the University of North Carolina at Chapel Hill reviewed medical records from 205 patients with EoE who underwent esophageal dilation. Of those, 26% received at least three dilations as either sole treatment for EoE or histologically refractory disease, undergoing a total of 408 dilations. They had previously failed to respond to proton pump inhibitors or steroids (75%), or had poor adherence to medication (40%) or preferred dilation (23%).
Compared with the routine-care group, who received two or fewer dilations or had histologic response to other treatments, patients in the dilation-only group were younger (41 vs. 33 years; P=0.003), had a smaller mean baseline esophageal diameter (11.5 vs. 9.8 mm; P=0.005) and underwent more dilations on average (3.4 vs. 7.7; P<0.001). They achieved a smaller final esophageal diameter (16.7 vs. 15.7 mm; P=0.01).
Fifty-seven percent of those undergoing dilation alone reported symptom response. The researchers observed no deaths or perforations resulting directly from dilations, but seven patients required hospitalization during follow-up for chest pain, inability to tolerate oral food or drink, or food impaction.
—Compiled and written by David Wild