SAN DIEGO—In a matched propensity analysis of almost 4,000 patients, glucagon-like peptide-1 receptor agonists appeared to protect patients with chronic pancreatitis from developing acute pancreatitis and other negative health-related outcomes, according to a study presented at DDW 2025.
“Across the board, for all outcomes—acute pancreatitis, all-cause mortality, hospitalizations, ICU admissions—we saw significant reductions in patients on GLP-1s compared to chronic pancreatitis patients not on these drugs,” said Mahmoud Y. Madi, MD, a senior fellow in gastroenterology and hepatology at Saint Louis University School of Medicine. “These findings suggest that GLP-1 therapy provides substantial benefits for managing type 2 diabetes in patients with chronic pancreatitis.”
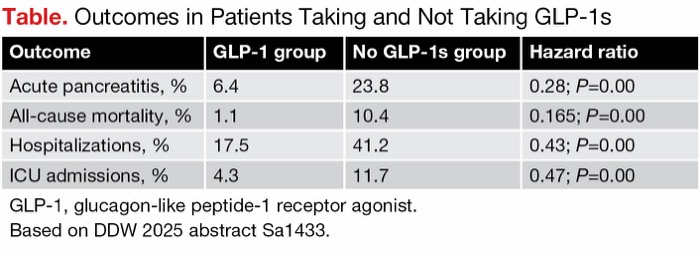
Patients with chronic pancreatitis taking GLP-1s were 72% less likely than those in the control group to develop acute pancreatitis. Acute pancreatitis developed in 6.4% of patients taking GLP-1s and 23.8% of nonusers (hazard ratio [HR], 0.28; P=0.00), Dr. Madi said (abstract Sa1433).
The reported incidence of acute pancreatitis among individuals with chronic pancreatitis “is a tricky question,” he added, as acute pancreatitis can be hard to accurately distinguish from other conditions. Studies have documented incidence rates ranging from about 15% to more than 30%, so a 6% rate reflects a large protective effect, he said.
“I think we have very strong data showing this,” Dr. Madi told Gastroenterology & Endoscopy News. “For patients with chronic pancreatitis and either type 2 diabetes or obesity, this could be a good class of medications to consider.”
As Dr. Madi noted, the increased use of GLP-1s has raised concerns about their safety profile, particularly regarding pancreatic adverse effects such as acute pancreatitis, in vulnerable populations. While these agents have proved effective in managing metabolic conditions, their impact on chronic pancreatitis remains unclear. This study evaluated the incidence of acute pancreatitis and other health outcomes in patients with chronic pancreatitis who were receiving GLP-1s, especially for type 2 diabetes.
In this retrospective cohort study, the investigators used the TriNetX database to identify adults with chronic pancreatitis and type 2 diabetes. Researchers identified 1,926 patients receiving GLP-1s for at least one year and propensity-matched them 1:1 with 1,926 chronic pancreatitis patients not on GLP-1s. The groups were well matched with respect to demographics, body mass index and comorbidities, although BMI was higher in patients taking GLP-1s (33 vs. 29 kg/m2; P<0.001). The study’s primary end point was the incidence of acute pancreatitis, and secondary outcomes included all-cause mortality, hospitalizations and ICU admissions.
In addition to the reduced incidence of acute pancreatitis, multiple other health benefits were observed among the GLP-1 cohort compared with controls, including decreased all-cause mortality, hospitalizations and ICU admissions (Table).
| Table. Outcomes in Patients Taking and Not Taking GLP-1s | |||
| Outcome | GLP-1 group | No GLP-1s group | Hazard ratio |
|---|---|---|---|
| Acute pancreatitis, % | 6.4 | 23.8 | 0.28; P=0.00 |
| All-cause mortality, % | 1.1 | 10.4 | 0.165; P=0.00 |
| Hospitalizations, % | 17.5 | 41.2 | 0.43; P=0.00 |
| ICU admissions, % | 4.3 | 11.7 | 0.47; P=0.00 |
| GLP-1, glucagon-like peptide-1 receptor agonist. Based on DDW 2025 abstract Sa1433. | |||
Dr. Madi added that more research is needed to explore the mechanisms behind the potential protective effect of these drugs in patients with chronic pancreatitis and to better understand their long-term effects.
Allison Yang, MD, the medical director of the pancreas program and a gastroenterologist at NewYork-Presbyterian Hospital/Weill Cornell Medical Center, in New York City, told Gastroenterology & Endoscopy News that the findings “are promising and would be exciting if they are true,” but said a randomized trial is required for confirmation and clinical application. While the use of propensity matching provides some measure of control, she said, questions remain about the accuracy of the acute pancreatitis diagnosis, compliance with the GLP-1 treatment and so forth. “Insurance coding only gives so much information,” she noted.
The reduction in risk for acute pancreatitis in chronic pancreatitis patients taking GLP-1s is “fairly significant,” Dr. Yang said, “but the study is retrospective, observational and relies on coding, so I think we should interpret the findings cautiously and hope to someday see a large-scale randomized trial.”
—Caroline Helwick
Drs. Madi and Yang reported no relevant financial disclosures.
This article is from the June 2025 print issue.