The COVID-19 pandemic’s hindrance of global and regional efforts to eliminate hepatitis C likely will result in more than 70,000 additional liver-related deaths by the year 2030, a study has found.
“When the COVID pandemic started, we didn’t really know what the full extent of disruptions was going to be across the spectrum of health care services,” said Sarah Blach, MHS, CPH, the HCV Group lead at the CDA Foundation in Boulder, Colo. “Hepatitis elimination is a fragile thing, so we want to make sure we’re not forgetting the fact that the pandemic will come to an end. What do we need to do next to make sure that we’re not losing the gains we’ve made for hepatitis?”
Ms. Blach and her colleagues assessed the potential effects on deaths and liver cancer associated with HCV using a series of mathematical models. These models evaluated the possible effect of delays in hepatitis elimination programs on hepatitis disease burden.
The researchers adapted previously developed models from 110 countries to include two different scenarios. One scenario modeled no delay in efforts to eliminate hepatitis. The other modeled a one-year delay, assuming significant disruption in screening, diagnosis and treatment interventions in the year 2020.
“At the time when we were doing this in April [2020], we didn’t really know the full extent of these disruptions,” Ms. Blach told Gastroenterology & Endoscopy News. “But using modeling, we were able to estimate what would happen if we were set back an entire year.”
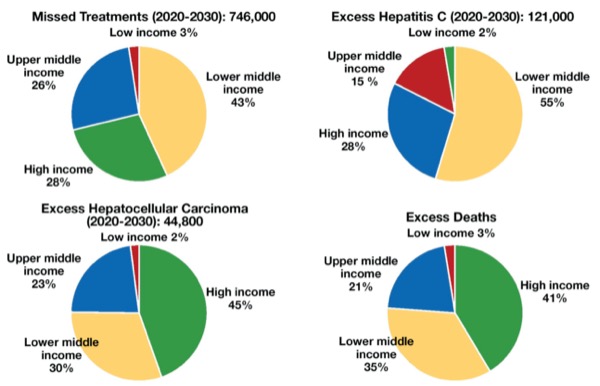
As reported in the Journal of Hepatology, in the no-delay scenario, approximately 1.1 million patients around the world were expected to be newly diagnosed in 2020, with about 1 million starting treatment. In the one-year delay scenario, none of these patients was diagnosed or treated (2021;74[1]:31-36).
The one-year delay scenario was found to result in 44,800 excess cases of hepatocellular carcinoma and 72,300 excess liver-related deaths. The analysis also found that most missed treatments would occur in lower- and middle-income countries, while most excess cases of hepatocellular carcinoma and liver-related deaths would occur in high-income countries.
An Opportunity for Change
As significant as these numbers are, they came as little surprise to the investigators. “We were actually thinking they might be a little higher,” Ms. Blach said. “One of the things we found was that because a lot of countries weren’t treating hepatitis at a particularly high level to begin with, the delay actually had a smaller effect than we were expecting in some places.”
Ms. Blach said she and her colleagues believe the findings present an opportunity for policymakers to prioritize hepatitis programs in the future.
“We can’t control certain things in public health,” she said. “Therefore, it’s important that we have strong hepatitis elimination programs in place at the country level that are resilient to these types of setbacks, since COVID-19 is likely not going to be the only setback we face in the future.”
Su Wang, MD, the president of the World Hepatitis Alliance, said the study offers a tangible idea of what may happen in the wake of the pandemic. “Of course, no model is ever going to be perfect, but these results give us a starting [point] to understand the impact of COVID-19 on hepatitis elimination,” she said.
Dr. Wang said the results may underestimate the ultimate increase in liver-related deaths born of COVID-19. “We never could have imagined [in March 2020], when everybody took two weeks off thinking that was going to be the extent of it,” she said. “But … the reality may actually be worse than we think.”
—Michael Vlessides
Dr. Wang and Ms. Blach reported no relevant financial disclosures. Financial support for the study was provided by the John C. Martin Foundation.
This article is from the June 2021 print issue.