In anticipation of an upcoming U.S. Supreme Court hearing that could have a drastic downstream effect on patient access to preventive services, the American College of Gastroenterology filed an amicus brief March 3 to alert the court about the importance of colorectal cancer screening.
The action follows the filing of a separate amicus brief by the American Society for Gastrointestinal Endoscopy (ASGE) and 32 other organizations, including the Crohn’s & Colitis Foundation, supporting all the preventive care recommendations of the U.S. Preventive Services Task Force (USPSTF), including those related to colonoscopy.
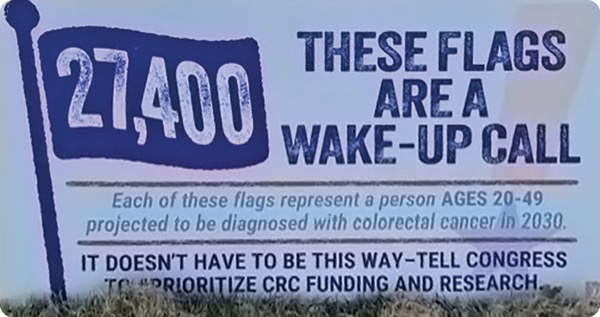
On March 9-11, gastroenterologists and other healthcare practitioners, as well as CRC survivors, caregivers and advocates traveled to Washington, D.C., to participate in Fight Colorectal Cancer’s Call-on Congress event. The event included panels and presentations, and many participants met with congressmembers to discuss the importance of CRC research and screening. Volunteers placed thousands of blue flags on the National Mall, each one representing one of the estimated 27,400 individuals aged 20 to 49 years who will be diagnosed with CRC in the year 2030 alone.
“CRC rates have fallen by nearly 50%, and that is likely the result of the heightened efforts focused on CRC screening and access, and removing the barrier of cost, which impacts everyone,” Amy Oxentenko, MD, a professor of medicine at Mayo Clinic, in Rochester, Minn., and the president of the ACG, told Gastroenterology & Endoscopy News.
“But even as we’re seeing decreased rates of CRC overall, we expect that by 2030, early-onset CRC will be a leading cause of death in patients 20 to 49,” Dr. Oxentenko said. “We would hate to lose the traction we have made with screening-eligible patients because we’ll need to continue our efforts with the younger population who will be in need of attention due to symptoms and a possible new diagnosis of CRC.”
Challenge to the Affordable Care Act
The case that initiated the filing of the brief started in 2022, when an employer group, the Braidwood group, challenged whether the preventive services mandate of the Affordable Care Act (ACA) was constitutional and whether it violated the Religious Freedom Restoration Act of 1993, Dr. Oxentenko said.
The ACG filed an amicus brief “because we felt it was really important for the court to understand how their decision may impact preventive services, and to be the voice of GI clinicians and their patients,” she added.
“These employers wanted to offer health insurance to employees that did not include certain preventative services mandated by the ACA that conflicted with certain personal and religious beliefs, such as contraception, [HIV prevention] and [human papillomavirus] vaccinations, among others,” she explained.
In 2023, a Texas district court agreed with Braidwood and invalidated any recommendations issued by the USPSTF after the date the ACA went into effect in 2010.
“That court cited that USPSTF members should be subject to a U.S. presidential nomination and Senate confirmation, which had not previously been done. The court concluded that because these members were ‘unconstitutionally appointed,’ their recommendations should not be used by Health and Human Services (HHS) to require insurance coverages of any services nationally,” Dr. Oxentenko said.
The Fifth Circuit Court of Appeals agreed last year that members of the USPSTF were not constitutionally appointed but also determined that the initial ruling went too far in invalidating all the task force’s recommendations.
In January 2025, the Supreme Court agreed to hear an appeal, and on Feb. 18, the Trump administration agreed to take over the case, arguing that the HHS secretary has ultimate oversight of the USPSTF members and its recommendations.
The Supreme Court plans to hear arguments on April 21 and is expected to issue a ruling later this spring.
CRC Screening and Prevention Are Not Controversial
“There is nothing controversial about CRC screening and prevention,” Dr. Oxentenko said. “CRC screening and prevention should be apolitical—where we all come together. We need to reduce barriers to care access, not create more, such that everyone has the opportunity to maintain health.”
The positive role of screening colonoscopy, in particular, is indisputable, noted Jason Dominitz, MD, a professor of medicine at the University of Washington School of Medicine, in Seattle, and the vice president of the ASGE. He highlighted an interim analysis of the NordICC study that showed screening reduces the actual incidence of CRC (N Engl J Med 2022;387(17):1547-1556).
“By doing screening colonoscopy, we prevent people from getting CRC. We want to do everything we can to encourage screening, and cost is a barrier. Right now, under the ACA, screening is fully covered, with no copay. If cost-sharing comes back, we fear that fewer patients will get screened, which would lead to some increase in cancer incidence, and there is a lot of cost associated with that,” Dr. Dominitz said.
At press time, the American Gastroenterological Association (AGA) had not filed an amicus brief, but Shazia Siddique, MD, MSHP, the chair of the AGA’s Government Affairs Committee, expressed the organization’s concern about the case in a statement provided to Gastroenterology & Endoscopy News. Dr. Siddique underscored that if the Supreme Court decides to rescind the current recommendations of the USPSTF and potentially the task force itself, patients likely will face significant barriers to CRC screening and insurance coverage. The AGA has worked with other organizations to make “notable strides in increasing screening rates to prevent the development of colorectal cancer. Despite this, colorectal cancer is expected to be the leading cause of cancer death in young Americans,” Dr. Siddique said. “This is a precarious moment in history, in which the court’s decision should not be taken lightly.”
—Monica J. Smith
This article is from the April 2025 print issue.