This month, my focus is on studies highlighting strategies to improve the quality of colonoscopy, including improving the adenoma detection rate (ADR), reducing bleeding after polypectomy and optimizing optical evaluation to predict invasive cancer in large non-pedunculated colorectal polyps (LNPCPs).
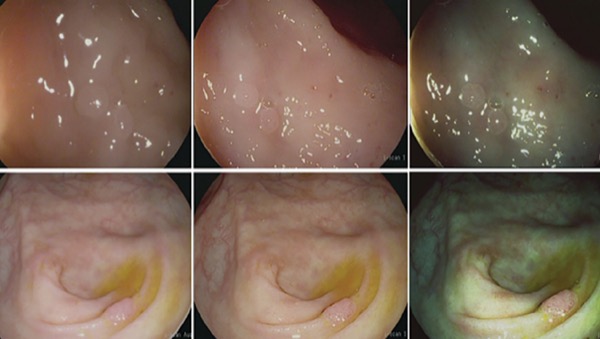
Colorectal polyps typically are evaluated by optical methods, including high-definition white light endoscopy and virtual chromoendoscopy. The first study I chose shows that successful optical evaluation is dependent on lesion morphology, and flat lesions can be evaluated efficiently by endoscopy to rule out submucosal invasion (SMI). Lesions larger than 2 cm, on the other hand, may be difficult to evaluate for SMI using optical techniques.
The second study is a systematic review and meta-analysis that addresses the question of whether prophylactic clipping should be routinely used after polyp resection. The results suggested that routine clipping does not reduce delayed bleeding after polyp resection. However, in patients with proximally located polyps, a polyp size of 2 cm or larger, and in those on anticoagulation or dual antiplatelet agents, prophylactic clipping is effective.
Finally, the authors of the third study evaluated whether the monitoring of withdrawal time or use of report cards for physicians affected ADR. They found that a physician colonoscopy quality report card, but not monitoring of withdrawal time, was associated with a significant improvement in ADR.
Is Optical Evaluation of LNPCPs Reliable?
(Clin Gastroenterol Hepatol 2021 May 12. https://doi.org/ 10.1016/ j.cgh.2021.05.017)
This analysis included 1,583 large (=2 cm) LNPCPs that were evaluated as part of a prospective, multicenter, observational cohort study. The median polyp size was 35 mm, and 855 were flat and 728 were nodular. Seven endoscopists with a median of 15 years of experience conducted the initial procedures and used established features, such as Kudo V pit pattern, depressed morphology, rigidity and fixation, and ulceration to determine the likelihood of submucosal invasive cancer (SMIC).
SMIC was observed in 9.2% (95% CI, 7.9%-10.8%) of the lesions, and the overall sensitivity and specificity of optical evaluation was 67.1% and 95.1%, with a high negative predictive value of 96.6%, according to the researchers. Overall, SMIC was missed in 3% (95% CI, 2.3%-4%) of lesions. SMIC was more likely to be missed in mixed lesions (5.2%) compared with granular (3.2%) or nongranular (2.2%) lesions.
Several variables independently predicted missed SMIC, including a polyp size of 4 cm or larger (odds ratio [OR], 2; 95% CI, 1-3.8), rectosigmoid location (OR, 2; 95% CI, 1.1-3.7) and nodular morphology (OR, 7.2; 95% CI, 2.8-18.9) (P<0.039 for all).
Consider Prophylactic Clipping for Specific Groups
(Clin Gastroenterol Hepatol 2021 May 2. https://doi.org/ 10.1016/ j.cgh.2021.05.012)
This meta-analysis included 13 studies looking at delayed bleeding within 30 days of prophylactic clipping after polypectomy of LNPCPs. The data included 5,380 patients who had 8,948 polyps resected and clipped.
Overall, prophylactic clipping led to no significant effect on delayed bleeding (OR, 0.94; 95% CI, 0.76-1.17), according to the researchers, although it reduced delayed bleeding for proximal polyps of 2 cm or larger (OR, 0.62; 95% CI, 0.44-0.88). The effect was greatest in patients receiving antithrombotic agents, in whom delayed bleeding decreased from 10.8% to 6.4% with prophylactic clipping (OR, 0.59; 95% CI, 0.35-0.99; number needed to treat [NNT], 23). Similarly, in patients receiving anticoagulants or double platelet inhibitors, delayed bleeding decreased from 14.6% to 6.3% when clips were applied prophylactically (OR, 0.40; 95% CI, 0.16-1.01; NNT, 12).
Physician Report Cards Increase ADRs
(2021 Virtual Digestive Disease Week; abstract Sa089)
The authors of this meta-analysis examined the impact of withdrawal time monitoring and physician report cards on ADRs. They included over 55,000 colonoscopies documented in 13 randomized controlled trials or observational studies published through 2018.
Physician report cards were associated with a 31% increase in ADRs (OR, 1.31; 95% CI, 1.15-1.5; P<0.0001), while slower withdrawal time did not increase ADRs (OR, 1.02; 95% CI, 0.86-1.22; P=0.81).
—Compiled and written by David Wild
This article is from the August 2021 print issue.