This month’s installment of “Expert Picks” is from Brooks D. Cash, MD, the chief of the Division of Gastroenterology, Hepatology and Nutrition at The University of Texas Health Science Center at Houston, and the Dan and Lillie Sterling Professor of Medicine at UTHealth Houston McGovern Medical School. Dr. Cash is the most recent chair of the ACG Educational Affairs Committee, and he coordinated the Scientific Committee for the 2022 annual meeting of the American College of Gastroenterology. Some of his favorite research from this year’s conference, specifically the innovations in esophageal and liver care, is detailed below.
Oral Presentation 14. Efficacy and safety of on-demand vonoprazan versus placebo in the treatment of heartburn in symptomatic nonerosive reflux disease (NERD) patients: a phase 2 randomized controlled trial (Fass et al)
Researchers led by Ronnie Fass, MD, MACG, from Case Western Reserve University, in Cleveland, investigated the use of vonoprazan (Takecab, Phathom) as an on-demand treatment for symptomatic nonerosive reflux disease.

The study was a phase 2, double-blind, placebo-controlled study that enrolled patients who have had recurrent heartburn episodes for at least four out of seven consecutive days over at least six months and had a normal endoscopy. After a four-week run-in period of 20 mg of vonoprazan once daily, responsive patients who were without heartburn for seven days were randomized 1:1:1:1 to receive placebo or 10, 20 or 40 mg of vonoprazan. Of the 458 patients enrolled, 207 were randomized. The primary end point was the percentage of heartburn episodes with complete relief (no heartburn within three hours) and sustained relief (no heartburn for at least 24 hours).
In the vonoprazan 10-, 20- and 40-mg groups, 56%, 60% and 70%, respectively, met the criteria for complete and sustained relief, versus 27.3% for placebo. Vonoprazan also appeared to be well tolerated, with more treatment-emergent adverse events occurring in the placebo group than in all three vonoprazan groups.
The researchers concluded that on-demand vonoprazan for episodic heartburn is efficacious and well tolerated and may be an attractive alternative to daily heartburn therapy.
Dr. Cash: This is a phase 2, randomized controlled trial of the first entrant into the U.S. market of a new class of acid-suppressing medications, potassium-competitive acid blockers (PCABs), that work differently than proton pump inhibitors and H2 blockers.
This study was pragmatic and important for two reasons: It evaluated vonoprazan in the heartburn population of patients who do not have erosive esophagitis, which is the largest population of patients with heartburn, and it evaluated the effects of vonoprazan as an on-demand therapy, which is a characteristic that our patients seem to really want. There appeared to be a dose response favoring vonoprazan, and all doses were superior to placebo, so these are encouraging early data that will shape phase 3 studies.
Patients want to take on-demand therapy because they often don’t have constant symptoms, and on-demand therapy with PPIs is not very effective. So, having a more robust on-demand therapy that gives rapid and prolonged symptom relief could be a real addition to our armamentarium.
The next step for this drug is a phase 3, placebo-controlled, randomized trial, and I think we all will eagerly await those results.
Oral Presentation 35. Cap assisted endoscopic treatment of esophageal food bolus and/or foreign body ingestion: a systematic review and meta-analysis (Mohan et al)
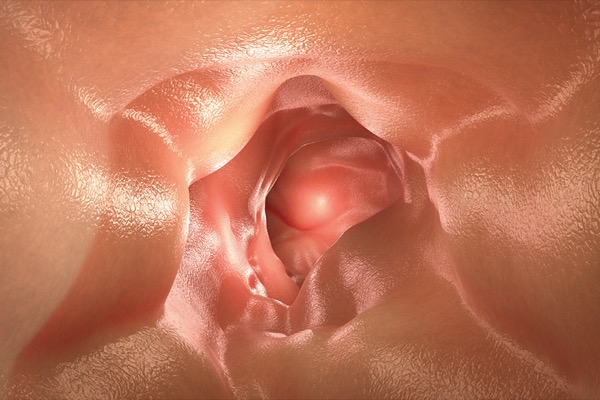
Early intervention and short procedure duration are associated with improved outcomes in patients with esophageal impaction. This meta-analysis by Mohan et al reported on pooled outcomes of cap-assisted endoscopic removal of food bolus and foreign bodies in the esophagus and evaluated whether outcomes were improved with cap assistance.
In the six studies included, 677 patients had cap-assisted endoscopy and 694 were treated with conventional methods. The pooled odds ratio (OR) for technical success was significant for the cap-assisted method (OR, 7.1; 95% CI, 1.9-26.9; P=0.004; heterogeneity measure [I2]=0). Outcomes were even better for en bloc removal (OR, 26.6; 95% CI, 17.6-40.2; P<0.001; I2=0). Procedure time was reduced by 4.6 minutes (95% CI, –6.5 to –2.8; P<0.001; I2=99) compared with the conventional method.
The cap-assisted method had better technical success with general anesthesia but was faster without general anesthesia. Pooled adverse events between traditional and cap-assisted endoscopy were comparable.
Dr. Cash: Esophageal food impactions are considered endoscopic emergencies, and they’re one of the classic indications for urgent endoscopy. While it isn’t a head-to-head comparison, this analysis showed cap-assisted endoscopy had a significantly higher odds of disimpaction success and for en bloc removal, which saves time and is safer than piecemeal disimpaction requiring multiple intubations or overtube placement. This is an interesting meta-analysis that supports the use of an endoscopic cap for foreign body removal, showing that it’s not only more effective, but it’s also more efficient.
I think this is an important finding that holds some promise for helping clinicians modify their current practices and potentially have better outcomes in the future with these often-difficult procedures.
Oral Presentation 9. Anticoagulation for the treatment of portal vein thrombosis in patients with cirrhosis: a systematic review and meta-analysis (Yao et al)
Yao et al from the University of California, Los Angeles David Geffen School of Medicine looked at anticoagulants as a treatment for portal vein thrombosis (PVT) in patients with cirrhosis in a systemic review and meta-analysis. Currently, consensus on anticoagulation use in this clinical setting is limited to symptomatic patients.
The review, which included 17 studies and nearly 1,500 patients, found that anticoagulation for PVT was associated with PVT improvement, PVT recanalization, decreased PVT progression and decreased mortality. Use of anticoagulation was not associated with an increase in bleeding events.
Improved outcomes and survival suggest that anticoagulation has clinical utility in PVT patients with cirrhosis. While a larger randomized controlled trial is needed, these findings could inform the development of modern clinical guidelines, the researchers noted.
Dr. Cash: PVT is a common complication that we see in patients with cirrhosis, especially in those with more advanced cirrhosis. But we typically only treat these patients with anticoagulation to dissolve the clot or promote blood flow through the portal vein when they’re symptomatic.
However, this study showed better outcomes, most importantly lower mortality without increased bleeding risk, with anticoagulation of cirrhotic patients with PVT, regardless of symptoms. While this is not a prospective head-to-head study, we have to recognize that this is a tough area to research and that these are tenuous patients with significant comorbidities. So, I think the current findings are provocative data that deserve additional investigation and have real potential to inform future practice in this area.
Oral Presentation 22. Terlipressin treatment of patients with hepatorenal syndrome type 1 decreased the need for renal replacement therapy in transplant recipients: a 12-month follow-up of the CONFIRM Study (Reddy et al)
Research has shown that terlipressin (Terlivaz, Mallinckrodt) can aid in reversing type 1 hepatorenal syndrome (HRS) and reduce the need for renal replacement therapy. In a follow-up to the CONFIRM study, Reddy et al investigated terlipressin’s impact on renal replacement therapy through 12 months after liver transplant.
A total of 300 patients with HRS were treated with terlipressin (n=199) or placebo (n=101) for up to 14 days. Renal replacement therapy included any procedure that replaced non-endocrine kidney function, including continuous hemofiltration and hemodialysis, intermittent hemodialysis, peritoneal dialysis, ultrafiltration, or other dialysis and filtration techniques.
In the terlipressin group, 46 patients (23%) received a liver transplant and three received a simultaneous liver–kidney transplant, compared with 29 (28%) and two patients in the placebo group.
Verified HRS reversal, defined as two consecutive serum creatine values of 1.5 mg/dL or less at least two hours apart, was comparable between the two groups. But HRS reversal, which was serum creatine of 1.5 mg/dL or less while receiving treatment by day of discharge, was significantly higher in the terlipressin group (P=0.021). The pretransplant need for renal replacement therapy also was significantly lower in the terlipressin group (P=0.007).
The researchers concluded that patients with HRS who received terlipressin and a liver transplant had a decreased need for renal replacement therapy for up to 12 months after transplantation.
Dr. Cash: HRS is a feared complication of decompensated liver disease. It’s heralded by worsening renal function, as well as worsening liver function, and is often a sign of progression toward mortality.
The real take-home message from this study is that terlipressin is a new therapy that appears to reduce the risk for needing renal replacement therapy in critically ill patients with HRS who are undergoing a liver transplant and that it can save resources and decrease complications in these already severely ill patients. There is some signal that there may be some overall survival benefit, too, but larger studies are needed to really tease that out.
Oral Presentation 68. Use of GLP1 agonists or SGLT2 inhibitors in non-alcoholic steatohepatitis patients with T2DM is associated with a lower risk of cirrhosis: a nationwide population-based study (Eltelbany et al)
Beyond lifestyle changes, treatment options for nonalcoholic steatohepatitis are limited. Some single-center studies have suggested type 2 diabetes treatments such as glucagon-like peptide-1 (GLP1) receptor agonists and sodium–glucose cotransporter-2 (SGLT2) inhibitors may be beneficial. This population-based study looked at the prevalence of cirrhosis in NASH patients with type 2 diabetes mellitus (T2DM) taking GLP1 agonists or SGLT2 inhibitors.
Eltelbany et al used the Explorys database, which includes 74 million unique patients across 300 U.S. hospitals. Patients over the age of 18 years with T2DM and NASH were identified. The researchers investigated the prevalence of cirrhosis in NASH patients with and without GLP1 agonists and SGLT2 inhibitor therapy, excluding other common causes of chronic liver disease.
Of the 29,000 NASH patients with T2DM, 17.5% received GLP1 agonists and 13.2% received SGLT2 inhibitors. The patients who received therapy were more likely to be white and younger than 65 years of age. Forty-three percent of the patients developed cirrhosis. Of note, GLP1 agonists or SGLT2 inhibitors were associated with a significantly lower risk for cirrhosis (OR, 0.83; 95% CI, 0.79-0.88). Subgroup analysis showed that patients who were receiving SGLT2 inhibitor therapy had the lowest risk for developing cirrhosis.
Dr. Cash: NASH and nonalcoholic fatty liver disease (NAFLD) are the most important causes, currently, of advanced liver failure and cirrhosis in the United States, but there’s no well-established standard of care for these conditions other than weight loss and managing comorbidities.
However, this study shows that use of either of two popular classes of diabetes medicines was associated with a significantly lower risk for cirrhosis—about a 17% lower risk. So, these are exciting data for an area that has been frustrating for clinicians to treat for many years.
Having evidence on the efficacy of medications that have already been shown to be safe and effective for other indications is also particularly exciting, since they have already run the gauntlet of FDA evaluation for those other indications and we are comfortable with their use. We need additional studies, as the researchers highlight, to determine which of these therapies may be the best to use in patients with NASH and NAFLD and to what degree they may actually decrease the risk for cirrhosis in these patients.
—Compiled and written by Donavyn Coffey
This article is from the January 2023 print issue.