WASHINGTON—Short myotomy was equivalent to long myotomy for the treatment of type I and type II achalasia, offering the benefit of shorter procedure time and less gastroesophageal reflux disease, according to the results of a single-center retrospective comparative study.
Over the past decade, peroral endoscopic myotomy (POEM) has evolved as a standard therapy for patients with achalasia because it allows for precise targeting, is more effective than pneumatic balloon dilation, and is as effective as and less invasive than laparoscopic Heller myotomy. However, POEM does have its pitfalls, including post-procedure gastroesophageal reflux disease and blown-out myotomy that results in treatment failure.
Given that considerable variations exist in the technique of POEM with respect to the length and orientation of the myotomy, Rishi Pawa, MD, the director of interventional endoscopy at Wake Forest Baptist Health, in Winston-Salem, N.C., and his co-investigators designed a study to compare the clinical outcomes of short versus long esophagomyotomy for type I and type II achalasia.
At DDW 2024, Dr. Pawa presented findings from the retrospective study of 50 consecutive patients undergoing POEM at his center from March 2019 to August 2023 (abstract 595). The investigators divided patients into two groups based on the length of the esophagomyotomy, with 25 undergoing short myotomy (3-4 cm) and 25 long myotomy (7-9 cm). Pre-POEM workup included high-resolution esophageal manometry, esophagogastroduodenoscopy with EndoFlip (Medtronic) and timed barium swallow. Baseline characteristics were similar between the groups, with the exception of higher Eckardt scores in the short myotomy group (9 vs. 7; P=0.039), Dr. Pawa noted.
All procedures were performed by a single endoscopist using a posterior approach. Post-POEM follow-up included an esophagram one day after the procedure to rule out a leak, as well as clinic visits at two weeks and one, three, six and 12 months. The patients received a proton pump inhibitor for four weeks. In addition, they underwent EGD with EndoFlip two to three months post-POEM as well as high-resolution esophageal manometry, timed barium swallow and a 24-hour pH impedance study six to 12 months after the procedure.
Clinical Outcomes Similar
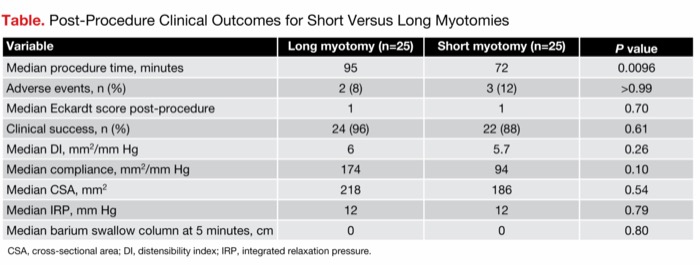
The median lengths of the myotomies were 4 cm in the short group and 8 cm in the long group. The length of gastric myotomy was 2 cm in each group. No significant differences in clinical outcomes were observed between the two POEM approaches (Table).
| Table. Post-Procedure Clinical Outcomes for Short Versus Long Myotomies | |||
| Variable | Long myotomy (n=25) | Short myotomy (n=25) | P value |
|---|---|---|---|
| Median procedure time, minutes | 95 | 72 | 0.0096 |
| Adverse events, n (%) | 2 (8) | 3 (12) | >0.99 |
| Median Eckardt score post-procedure | 1 | 1 | 0.70 |
| Clinical success, n (%) | 24 (96) | 22 (88) | 0.61 |
| Median DI, mm2/mm Hg | 6 | 5.7 | 0.26 |
| Median compliance, mm2/mm Hg | 174 | 94 | 0.10 |
| Median CSA, mm2 | 218 | 186 | 0.54 |
| Median IRP, mm Hg | 12 | 12 | 0.79 |
| Median barium swallow column at 5 minutes, cm | 0 | 0 | 0.80 |
| CSA, cross-sectional area; DI, distensibility index; IRP, integrated relaxation pressure. | |||
“Median procedure time was much shorter for patients undergoing a short myotomy, and clinical success was similar for both groups,” Dr. Pawa reported. Other clinical parameters were comparable. More adverse events were seen after long myotomy, but the differences were not statistically significant. In particular, for long versus short myotomies, median follow-up was 533 and 339 days, respectively (P=0.20), during which time GERD was observed in 40% and 32% (P=0.77) and reflux esophagitis in 28% and 12% (P=0.29).
Dr. Pawa commented that his group is “routinely doing short myotomy for type I and type II achalasia, given that it’s clinically equivalent to long myotomy, with an additional benefit of reduced operating time.”
Joseph R. Triggs, MD, PhD, an assistant professor of medicine at Fox Chase Cancer Center, in Philadelphia, said the findings clearly support short myotomy. “At its core, treatment for achalasia aims to disrupt the abnormally hypertensive lower esophageal sphincter, which is 3 to 4 cm in length, to allow the passage of food into the stomach. However, historically, both Heller myotomy and POEM have cut 6 to 8 cm of muscle in the esophagus. Using in silico modeling, we were previously able to show shorter myotomies reduce the risk of developing blown-out myotomy, which has been associated with worse outcomes [Gastrointest Endosc 2021;93(4):861-868.e1]. This study now supports the recommendation that shorter myotomies for types I and II achalasia may reduce the risk of long-term complications without a loss in efficacy.”
—Caroline Helwick
Dr. Pawa reported a financial relationship with Boston Scientific and Cook. Dr. Triggs reported no relevant financial disclosures.
This article is from the October 2024 print issue.